| Reference | [1]. N Engl J Med. 2021 Jan 28;384(4):325-334. doi: 10.1056/NEJMoa2008470. Epub 2021 Jan 13.<br />
Inhaled Treprostinil in Pulmonary Hypertension Due to Interstitial Lung Disease.<br />
Waxman A(1), Restrepo-Jaramillo R(1), Thenappan T(1), Ravichandran A(1), Engel P(1), Bajwa A(1), Allen R(1), Feldman J(1), Argula R(1), Smith P(1), Rollins K(1), Deng C(1), Peterson L(1), Bell H(1), Tapson V(1), Nathan SD(1).<br />
Author information: (1)From Brigham and Women's Hospital, Boston (A.W.); the University of South Florida, Tampa (R.R.-J.), and St. Vincent's Lung, Sleep, and Critical Care Specialists, Jacksonville (A.B.) – both in FL; the University of Minnesota, Minneapolis (T.T.); St. Vincent Medical Group, Indianapolis (A.R.); the Carl and Edyth Lindner Research Center at the Christ Hospital, Cincinnati (P.E.); University of California Davis Medical Center, Sacramento (R. Allen), and Cedars-Sinai, Los Angeles (V.T.); Arizona Pulmonary Specialists, Phoenix (J.F.); the Medical University of South Carolina, Charleston (R. Argula); United Therapeutics Corporation, Silver Spring, MD (P.S., K.R., C.D., L.P., H.B.); and Inova Fairfax Hospital, Falls Church, VA (S.D.N.).<br />
Comment in N Engl J Med. 2021 Jan 28;384(4):376-377. N Engl J Med. 2021 May 13;384(19):1869. N Engl J Med. 2021 May 13;384(19):1869-1870. N Engl J Med. 2021 May 13;384(19):1870. N Engl J Med. 2021 May 13;384(19):1870-1871. N Engl J Med. 2021 May 13;384(19):1871.<br />
BACKGROUND: No therapies are currently approved for the treatment of pulmonary hypertension in patients with interstitial lung disease. The safety and efficacy of inhaled treprostinil for patients with this condition are unclear. METHODS: We enrolled patients with interstitial lung disease and pulmonary hypertension (documented by right heart catheterization) in a multicenter, randomized, double-blind, placebo-controlled, 16-week trial. Patients were assigned in a 1:1 ratio to receive inhaled treprostinil, administered by means of an ultrasonic, pulsed-delivery nebulizer in up to 12 breaths (total, 72 μg) four times daily, or placebo. The primary efficacy end point was the difference between the two groups in the change in peak 6-minute walk distance from baseline to week 16. Secondary end points included the change in N-terminal pro-B-type natriuretic peptide (NT-proBNP) level at week 16 and the time to clinical worsening. RESULTS: A total of 326 patients underwent randomization, with 163 assigned to inhaled treprostinil and 163 to placebo. Baseline characteristics were similar in the two groups. At week 16, the least-squares mean difference between the treprostinil group and the placebo group in the change from baseline in the 6-minute walk distance was 31.12 m (95% confidence interval [CI], 16.85 to 45.39; P<0.001). There was a reduction of 15% in NT-proBNP levels from baseline with inhaled treprostinil as compared with an increase of 46% with placebo (treatment ratio, 0.58; 95% CI, 0.47 to 0.72; P<0.001). Clinical worsening occurred in 37 patients (22.7%) in the treprostinil group as compared with 54 patients (33.1%) in the placebo group (hazard ratio, 0.61; 95% CI, 0.40 to 0.92; P = 0.04 by the log-rank test). The most frequently reported adverse events were cough, headache, dyspnea, dizziness, nausea, fatigue, and diarrhea. CONCLUSIONS: In patients with pulmonary hypertension due to interstitial lung disease, inhaled treprostinil improved exercise capacity from baseline, assessed with the use of a 6-minute walk test, as compared with placebo. (Funded by United Therapeutics; INCREASE ClinicalTrials.gov number, NCT02630316.).<br />
DOI: 10.1056/NEJMoa2008470 PMID: 33440084 [Indexed for MEDLINE]<br />
<br />
[2]. Am J Respir Crit Care Med. 2020 Mar 15;201(6):707-717. doi: 10.1164/rccm.201908-1640OC.<br />
Combination Therapy with Oral Treprostinil for Pulmonary Arterial Hypertension. A Double-Blind Placebo-controlled Clinical Trial.<br />
White RJ(1), Jerjes-Sanchez C(2), Bohns Meyer GM(3), Pulido T(4), Sepulveda P(5), Wang KY(6), Grünig E(7), Hiremath S(8), Yu Z(9), Gangcheng Z(10), Yip WLJ(11), Zhang S(12), Khan A(13), Deng CQ(14), Grover R(14), Tapson VF(15); FREEDOM-EV Investigators.<br />
Collaborators: Svetliza GN, Lescano AJ, Bortman GR, Diez FA, Botta CE, Fitzgerald J, Feenstra E, Kermeen FD, Keogh AM, Williams TJ, Yousseff PP, Ng BJ, Smallwood DM, Dwyer NB, Brown MR, Lang IM, Steringer-Mascherbauer R, Arakaki JSO, Campos FTAF, de Amorim Correa R, de Souza R, Bohns Meyer GM, Moreira MAC, Yoo HHB, Lapa MS, Swiston J, Hirani N, Mehta S, Michelakis E, Sepulveda PA, Blancaire MMZ, Liu J, Shuyang Z, Pan L, Chunde B, Qun Y, Xiaoshu C, Zaixin Y, Li X, Hua Y, Gangcheng Z, Zhu X, Chen Y, Zhaozhong C, Yang Y, Daxin Z, Jieyan S, Nielsen-Kudsk JE, Carlsen J, Bourdin A, Hachulla E, Dromer C, Chaouat A, Reynaud-Gauber M, Seronde MF, Klose H, Halank M, Hoffken G, Ewert R, Rosenkranz S, Grunig E, Kruger U, Kronsbein J, Hauptmeier BM, Koch A, Held M, Lange TJ, Neurohr C, Wilkens H, Wilhelm Wirtz HR, Konstantinides S, Argyropoulou-Pataka P, Orfanos S, Hiremath S, Kerkar PG, Suresh PV, Baxi HA, Oomman A, Abhaichand RK, Arjun PKE, Chopra V, Mehrotra R, Rajput RK, Sawhney JPS, Bimalendu S, Sharma KH, Sastry BKS, Kramer MR, Segel MJ, Ben-Dov I, Berkman N, Yigla M, Adir Y, D'Alto M, Vizza CD, Scelsi L, Vitulo P, Pulido TR, Jerjes-Sanchez C, Boonstra A, Vonk MC, Sobkowicz B, Mularek-Kubzdela T, Torbicki A, Podolec P, Teik LS, Yip WLJ, Chang HJ, Kim HK, Park JB, Chang SA, Kim DK, Chang SA, Chung WJ, Song JM, Nissell M, Hjalmarsson C, Rundqvist B, Huang WC, Cheng CC, Hsu CH, Hsu HH, Wang KY, Coghlan JG, Kiely DG, Pepke-Zaba JW, Lordan JL, Corris PA, Cadaret L, Hansdottir S, Oudiz RJ, Badesch DB, Mathier M, Schilz R, Hill N, Waxman A, Markin CJ, Zwicke DL, Fisher M, Franco V, Sood N, Park MH, Allen R, Feldman JP, Balasubramanian V, Seeram VK, Bajwa A, Thompson AB 3rd, Migliore C, Elwing J, McConnell JW, Mehta JP, Rahaghi FF, Rame JE, Khan A, Patel B, Oren RM, Klinger JR, Alnuaimat H, Allen S, Harvey W, Eggert MS, Hage A, Miller CE, Awdish RLA, Cajigas H, Grinnan D, Trichon BH, McDonough C, White RJ, Rischard F.<br />
Author information: (1)Division of Pulmonary and Critical Care Medicine and the Mary M. Parkes Center, University of Rochester Medical Center, Rochester, New York. (2)Unidad de Investigación Clínica en Medicina, Monterrey, Mexico. (3)Complexo Hospitalar Santa Casa de Porto Alegre, Porto Alegre, Brazil. (4)Departamento de Cardioneumología, Instituto Nacional de Cardiología Ignacio Chávez, Mexico City, Mexico. (5)Pontifica Universidad Católica de Chile, Santiago, Chile. (6)Taichung Veterans General Hospital, Taichung, Taiwan. (7)Thoraxclinic at University Hospital Heidelberg, Heidelberg, Germany. (8)Ruby Hall Clinic, Grant Medical Foundation, Pune, India. (9)Department of Cardiology, Xiangya Hospital of Central South University, Changsha, China. (10)Wuhan Asia Heart Hospital, Wuhan Shi, China. (11)Department of Cardiology, National University Heart Centre, Singapore, Singapore. (12)Peking Union Medical College Hospital, Beijing, China. (13)Oregon Health and Science University, Portland, Oregon. (14)United Therapeutics, Research Triangle Park, North Carolina; and. (15)Division of Pulmonary and Critical Care Medicine, Cedars Sinai Medical Center, Los Angeles, California.<br />
Comment in Am J Respir Crit Care Med. 2020 Mar 15;201(6):647-649.<br />
Rationale: Oral treprostinil improves exercise capacity in patients with pulmonary arterial hypertension (PAH), but the effect on clinical outcomes was unknown.Objectives: To evaluate the effect of oral treprostinil compared with placebo on time to first adjudicated clinical worsening event in participants with PAH who recently began approved oral monotherapy.Methods: In this event-driven, double-blind study, we randomly allocated 690 participants (1:1 ratio) with PAH to receive placebo or oral treprostinil extended-release tablets three times daily. Eligible participants were using approved oral monotherapy for over 30 days before randomization and had a 6-minute-walk distance 150 m or greater. The primary endpoint was the time to first adjudicated clinical worsening event: death; hospitalization due to worsening PAH; initiation of inhaled or parenteral prostacyclin therapy; disease progression; or unsatisfactory long-term clinical response.Measurements and Main Results: Clinical worsening occurred in 26% of the oral treprostinil group compared with 36% of placebo participants (hazard ratio, 0.74; 95% confidence interval, 0.56-0.97; P = 0.028). Key measures of disease status, including functional class, Borg dyspnea score, and N-terminal pro-brain natriuretic peptide, all favored oral treprostinil treatment at Week 24 and beyond. A noninvasive risk stratification analysis demonstrated that oral treprostinil-assigned participants had a substantially higher mortality risk at baseline but achieved a lower risk profile from Study Weeks 12-60. The most common adverse events in the oral treprostinil group were headache, diarrhea, flushing, nausea, and vomiting.Conclusions: In participants with PAH, addition of oral treprostinil to approved oral monotherapy reduced the risk of clinical worsening.Clinical trial registered with www.clinicaltrials.gov (NCT01560624).<br />
DOI: 10.1164/rccm.201908-1640OC PMCID: PMC7068822 PMID: 31765604 [Indexed for MEDLINE]<br />
<br />
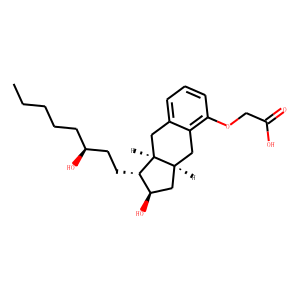
[3]. Treprostinil.<br />
Zare P(1), Heller D(1).<br />
In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan–. 2021 Jul 18.<br />
Author information: (1)Aventura Hospital and Medical Center<br />
Treprostinil is a medication used in the management and treatment of pulmonary arterial hypertension (PH). This activity outlines and reviews the indications, action, and contraindications for treprostinil as a valuable agent in treating PH. This activity will highlight the mechanism of action, adverse event profile, and other key factors pertinent to members of the interprofessional team in the management of patients with PH.<br />
PMID: 31424736<br />
<br />
[4]. Treprostinil.<br />
Drugs and Lactation Database (LactMed) [Internet]. Bethesda (MD): National Library of Medicine (US); 2006–. 2021 Apr 17.<br />
One patient taking treprostinil breastfed her infant for one year without any complications. However, until more data are available, treprostinil should only be used with careful monitoring during breastfeeding.<br />
PMID: 30000980<br />
<br />
[5]. Arterioscler Thromb Vasc Biol. 2020 Jun;40(6):1543-1558. doi: 10.1161/ATVBAHA.119.313883. Epub 2020 Apr 9.<br />
Treatment With Treprostinil and Metformin Normalizes Hyperglycemia and Improves Cardiac Function in Pulmonary Hypertension Associated With Heart Failure With Preserved Ejection Fraction.<br />
Wang L(1)(2), Halliday G(3), Huot JR(4), Satoh T(1)(5), Baust JJ(1), Fisher A(3), Cook T(3), Hu J(1), Avolio T(1), Goncharov DA(1), Bai Y(3), Vanderpool RR(6), Considine RV(7), Bonetto A(4), Tan J(8), Bachman TN(1), Sebastiani A(1), McTiernan CF(1), Mora AL(1)(8), Machado RF(3), Goncharova EA(1)(8), Gladwin MT(1)(8), Lai YC(3)(9).<br />
Author information: (1)From the Pittsburgh Heart, Lung, Blood and Vascular Medicine Institute (L.W., T.S., J.J.B., J.H., T.A., D.A.G., T.N.B., A.S., C.F.M., A.L.M., E.A.G., M.T.G.), University of Pittsburgh, PA. (2)The Third Xiangya Hospital, Central South University, Changsha, Hunan, China (L.W.). (3)Division of Pulmonary, Critical Care, Sleep and Occupational Medicine (G.H., A.F., T.C., Y.B., R.F.M., Y.-C.L.), Indiana University School of Medicine, Indianapolis. (4)Department of Surgery (J.R.H., A.B.), Indiana University School of Medicine, Indianapolis. (5)Department of Cardiovascular Medicine, Tohoku University Graduate School of Medicine, Sendai, Japan (T.S.). (6)Division of Translational and Regenerative Medicine, University of Arizona, Tucson (R.R.V.). (7)Division of Endocrinology (R.V.C.), Indiana University School of Medicine, Indianapolis. (8)Division of Pulmonary, Allergy and Critical Care Medicine (J.T., A.L.M., E.A.G., M.T.G.), University of Pittsburgh, PA. (9)Department of Anatomy, Cell Biology & Physiology (Y.-C.L.), Indiana University School of Medicine, Indianapolis.<br />
Comment in Arterioscler Thromb Vasc Biol. 2020 Sep;40(9):e260-e261. Arterioscler Thromb Vasc Biol. 2020 Oct;40(10):e273.<br />
OBJECTIVE: Pulmonary hypertension (PH) due to left heart disease (group 2), especially in the setting of heart failure with preserved ejection fraction (HFpEF), is the most common cause of PH worldwide; however, at present, there is no proven effective therapy available for its treatment. PH-HFpEF is associated with insulin resistance and features of metabolic syndrome. The stable prostacyclin analog, treprostinil, is an effective and widely used Food and Drug Administration-approved drug for the treatment of pulmonary arterial hypertension. While the effect of treprostinil on metabolic syndrome is unknown, a recent study suggests that the prostacyclin analog beraprost can improve glucose intolerance and insulin sensitivity. We sought to evaluate the effectiveness of treprostinil in the treatment of metabolic syndrome-associated PH-HFpEF. Approach and Results: Treprostinil treatment was given to mice with mild metabolic syndrome-associated PH-HFpEF induced by high-fat diet and to SU5416/obese ZSF1 rats, a model created by the treatment of rats with a more profound metabolic syndrome due to double leptin receptor defect (obese ZSF1) with a vascular endothelial growth factor receptor blocker SU5416. In high-fat diet-exposed mice, chronic treatment with treprostinil reduced hyperglycemia and pulmonary hypertension. In SU5416/Obese ZSF1 rats, treprostinil improved hyperglycemia with similar efficacy to that of metformin (a first-line drug for type 2 diabetes mellitus); the glucose-lowering effect of treprostinil was further potentiated by the combined treatment with metformin. Early treatment with treprostinil in SU5416/Obese ZSF1 rats lowered pulmonary pressures, and a late treatment with treprostinil together with metformin improved pulmonary artery acceleration time to ejection time ratio and tricuspid annular plane systolic excursion with AMPK (AMP-activated protein kinase) activation in skeletal muscle and the right ventricle. CONCLUSIONS: Our data suggest a potential use of treprostinil as an early treatment for mild metabolic syndrome-associated PH-HFpEF and that combined treatment with treprostinil and metformin may improve hyperglycemia and cardiac function in a more severe disease.<br />
DOI: 10.1161/ATVBAHA.119.313883 PMCID: PMC7255946 PMID: 32268788 [Indexed for MEDLINE]
|