| Reference | [1]. Lancet Infect Dis. 2019 Dec;19(12):1299-1311. doi: 10.1016/S1473-3099(19)30403-7. Epub 2019 Sep 25.<br />
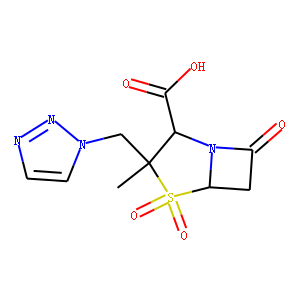
Ceftolozane-tazobactam versus meropenem for treatment of nosocomial pneumonia (ASPECT-NP): a randomised, controlled, double-blind, phase 3, non-inferiority trial.<br />
Kollef MH(1), Nováček M(2), Kivistik Ü(3), Réa-Neto Á(4), Shime N(5), Martin-Loeches I(6), Timsit JF(7), Wunderink RG(8), Bruno CJ(9), Huntington JA(9), Lin G(9), Yu B(9), Butterton JR(9), Rhee EG(10).<br />
Author information: (1)Washington University School of Medicine, St Louis, MO, USA. (2)General Hospital of Kolin, Kolin, Czech Republic. (3)North Estonia Medical Centre, Tallinn, Estonia. (4)Universidade Federal do Paraná, Curitiba, Brazil. (5)Hiroshima University, Hiroshima, Japan. (6)St James's Hospital, Dublin, Ireland; Universitat de Barcelona, Instituto de Investigaciones Biomédicas August Pi i Sunyer, Centro de Investigación Biomédica en Red Enfermedades Respiratorias, Barcelona, Spain. (7)Université Paris Diderot, Paris, France. (8)Northwestern University Feinberg School of Medicine, Chicago, IL, USA. (9)Merck & Co, Kenilworth, NJ, USA. (10)Merck & Co, Kenilworth, NJ, USA. Electronic address: [email protected].<br />
Comment in Lancet Infect Dis. 2019 Dec;19(12):1266-1267. Lancet Infect Dis. 2020 Jan;20(1):20-21. Lancet Infect Dis. 2020 Jan;20(1):20.<br />
BACKGROUND: Nosocomial pneumonia due to antimicrobial-resistant pathogens is associated with high mortality. We assessed the efficacy and safety of the combination antibacterial drug ceftolozane-tazobactam versus meropenem for treatment of Gram-negative nosocomial pneumonia. METHODS: We conducted a randomised, controlled, double-blind, non-inferiority trial at 263 hospitals in 34 countries. Eligible patients were aged 18 years or older, were undergoing mechanical ventilation, and had nosocomial pneumonia (either ventilator-associated pneumonia or ventilated hospital-acquired pneumonia). Patients were randomly assigned (1:1) with block randomisation (block size four), stratified by type of nosocomial pneumonia and age (<65 years vs ≥65 years), to receive either 3 g ceftolozane-tazobactam or 1 g meropenem intravenously every 8 h for 8-14 days. The primary endpoint was 28-day all-cause mortality (at a 10% non-inferiority margin). The key secondary endpoint was clinical response at the test-of-cure visit (7-14 days after the end of therapy; 12·5% non-inferiority margin). Both endpoints were assessed in the intention-to-treat population. Investigators, study staff, patients, and patients' representatives were masked to treatment assignment. Safety was assessed in all randomly assigned patients who received study treatment. This trial was registered with ClinicalTrials.gov, NCT02070757. FINDINGS: Between Jan 16, 2015, and April 27, 2018, 726 patients were enrolled and randomly assigned, 362 to the ceftolozane-tazobactam group and 364 to the meropenem group. Overall, 519 (71%) patients had ventilator-associated pneumonia, 239 (33%) had Acute Physiology and Chronic Health Evaluation II scores of at least 20, and 668 (92%) were in the intensive care unit. At 28 days, 87 (24·0%) patients in the ceftolozane-tazobactam group and 92 (25·3%) in the meropenem group had died (weighted treatment difference 1·1% [95% CI -5·1 to 7·4]). At the test-of-cure visit 197 (54%) patients in the ceftolozane-tazobactam group and 194 (53%) in the meropenem group were clinically cured (weighted treatment difference 1·1% [95% CI -6·2 to 8·3]). Ceftolozane-tazobactam was thus non-inferior to meropenem in terms of both 28-day all-cause mortality and clinical cure at test of cure. Treatment-related adverse events occurred in 38 (11%) of 361 patients in the ceftolozane-tazobactam group and 27 (8%) of 359 in the meropenem group. Eight (2%) patients in the ceftolozane-tazobactam group and two (1%) in the meropenem group had serious treatment-related adverse events. There were no treatment-related deaths. INTERPRETATION: High-dose ceftolozane-tazobactam is an efficacious and well tolerated treatment for Gram-negative nosocomial pneumonia in mechanically ventilated patients, a high-risk, critically ill population. FUNDING: Merck & Co.<br />
DOI: 10.1016/S1473-3099(19)30403-7 PMID: 31563344 [Indexed for MEDLINE]<br />
<br />
[2]. Clin Infect Dis. 2020 Jul 11;71(2):304-310. doi: 10.1093/cid/ciz816.<br />
Ceftolozane/Tazobactam vs Polymyxin or Aminoglycoside-based Regimens for the Treatment of Drug-resistant Pseudomonas aeruginosa.<br />
Pogue JM(1), Kaye KS(2), Veve MP(3), Patel TS(4), Gerlach AT(5), Davis SL(6), Puzniak LA(7), File TM(8), Olson S(9), Dhar S(10), Bonomo RA(11), Perez F(11).<br />
Author information: (1)Department of Clinical Pharmacy, University of Michigan College of Pharmacy, Ann Arbor, Michigan. (2)Division of Infectious Diseases, University of Michigan Medical School, Ann Arbor, Michigan. (3)Department of Clinical Pharmacy and Translational Science, University of Tennessee College of Pharmacy, Nashville, Tennessee. (4)Department of Pharmacy Services, Michigan Medicine, Ann Arbor, Michigan. (5)Department of Pharmacy Services, the Ohio State University Wexner Medical Center, Columbus, Ohio. (6)Department of Pharmacy, Henry Ford Hospital, Ann Arbor, Michigan; College of Pharmacy and Health Sciences, Wayne State University, Detroit, Michigan. (7)Merck & Co, Inc, Kenilworth, New Jersey. (8)Division of Infectious Diseases Summa Health, Northeast Ohio Medical University, Rootstown, Ohio. (9)Department of Pharmacy, Sinai Grace Hospital; Detroit Medical Center, Detroit, Michigan. (10)Department of Internal Medicine, Detroit Medical Center, Wayne State University School of Medicine, Michigan. (11)Division of Infectious Diseases and HIV Medicine, Louis Stokes Cleveland VA Medical Center, Case Western Reserve University School of Medicine, Cleveland, Ohio.<br />
Comment in Clin Infect Dis. 2020 Oct 23;71(7):1801-1802. Clin Infect Dis. 2020 Oct 23;71(7):1799-1801.<br />
BACKGROUND: Ceftolozane/tazobactam is a novel cephalosporin/beta-lactamase inhibitor combination that often retains activity against resistant Pseudomonas aeruginosa. The comparative safety and efficacy vs polymyxins or aminoglycosides in this setting remains unknown. METHODS: A retrospective, multicenter, observational cohort study was performed. Patients who received ceftolozane/tazobactam were compared with those treated with either polymyxin or aminoglycoside-based regimens for infections due to drug-resistant P. aeruginosa. Multivariate logistic regression was performed controlling for factors associated with treatment to assess the independent impact of ceftolozane/tazobactam on clinical cure, acute kidney injury (AKI), and in-hospital mortality. RESULTS: A total of 200 patients were included (100 in each treatment arm). The cohort represented an ill population with 69% in the intensive care unit, 63% mechanically ventilated, and 42% in severe sepsis or septic shock at infection onset. The most common infection type was ventilator-associated pneumonia (52%); 7% of patients were bacteremic. Combination therapy was more commonly used in polymyxin/aminoglycoside patients than those who received ceftolozane/tazobactam (72% vs 15%, P < .001). After adjusting for differences between groups, receipt of ceftolozane/tazobactam was independently associated with clinical cure (adjusted odds ratio [aOR], 2.63; 95% confidence interval [CI], 1.31-5.30) and protective against AKI (aOR, 0.08; 95% CI, 0.03-0.22). There was no difference in in-hospital mortality. The number needed to treat for a clinical cure with ceftolozane/tazobactam was 5, and the number needed to harm with AKI with a polymyxin/aminoglycoside was 4. CONCLUSIONS: These data support the preferential use of ceftolozane/tazobactam over polymyxins or aminoglycosides for drug-resistant P. aeruginosa infections.<br />
DOI: 10.1093/cid/ciz816 PMID: 31545346 [Indexed for MEDLINE]<br />
<br />
[3]. Crit Care Med. 2018 Jul;46(7):e725. doi: 10.1097/CCM.0000000000003115.<br />
Piperacillin-Tazobactam: Extended Infusion Versus Continuous Infusion.<br />
Messori A(1), Tulli G, Caccese E, Trippoli S, Marinai C.<br />
Author information: (1)HTA Unit, ESTAR, Regional Health Service, Firenze, Italy; Regional Health Agency of Tuscany, Firenze, Italy; HTA Unit, ESTAR, Regional Health Service, Firenze, Italy.<br />
Comment in Crit Care Med. 2018 Jul;46(7):e725-e726.<br />
Comment on Crit Care Med. 2018 Feb;46(2):236-243.<br />
DOI: 10.1097/CCM.0000000000003115 PMID: 29912125 [Indexed for MEDLINE]<br />
<br />
[4]. Clin Infect Dis. 2020 Nov 5;71(8):e331-e337. doi: 10.1093/cid/ciz1205.<br />
Is Piperacillin-Tazobactam Effective for the Treatment of Pyelonephritis Caused by Extended-Spectrum β-Lactamase-Producing Organisms?<br />
Sharara SL(1), Amoah J(2), Pana ZD(3), Simner PJ(4), Cosgrove SE(1), Tamma PD(2).<br />
Author information: (1)The Johns Hopkins University School of Medicine, Department of Medicine, Baltimore, Maryland, USA. (2)The Johns Hopkins University School of Medicine, Department of Pediatrics, Baltimore, Maryland, USA. (3)European University of Cyprus, Department of Medicine, Nicosia, Cyprus. (4)The Johns Hopkins University School of Medicine, Department of Pathology, Baltimore, Maryland, USA.<br />
Comment in Clin Infect Dis. 2020 Dec 3;71(9):2538-2539. Clin Infect Dis. 2020 Dec 3;71(9):2539-2540. Clin Infect Dis. 2020 Dec 3;71(9):2540-2541.<br />
BACKGROUND: Limited data exist regarding the efficacy of piperacillin-tazobactam (TZP) for the management of nonbacteremic pyelonephritis caused by extended-spectrum β-lactamase (ESBL)-producing organisms. METHODS: We conducted a multicenter observational study comparing clinical outcomes of adults hospitalized with ESBL-producing pyelonephritis who were receiving TZP versus carbapenems, using an inverse probability of treatment weighted propensity score analysis. Patients were eligible for inclusion if all of the following criteria were met: (1) urine cultures growing Escherichia coli, Klebsiella pneumoniae, Klebsiella oxytoca, or Proteus mirabilis at ≥50 000 colony-forming units/mL; (2) identification of an ESBL gene; (3) pyuria (≥10 white blood cells per high powered field in the urine); and (4) dysuria and fever plus at least 1 of the following symptoms: emesis, rigors, hypotension, or flank pain. RESULTS: There were 186 patients included in the propensity score-weighted cohort; 45 (24%) received TZP and 141 (76%) received a carbapenem. Of these 186 patients, 27% were admitted to the intensive care unit, 48% were immunocompromised, and 45% had underlying urologic abnormalities. There were no differences between the 2 groups in the proportion of patients (20% vs 25%) with recurrent cystitis or pyelonephritis with the same ESBL-producing organism within 30 days (odds ratio, 0.75; 95% confidence interval, .31-1.81; P = .52). There were no differences in the resolution of clinical symptoms by Day 7 or in 30-day mortality. There was 1 (2%) patient in the TZP arm and 11 (8%) patients in the carbapenem arm who had incident carbapenem-resistant organisms isolated within 30 days (P = .09). CONCLUSIONS: TZP may be a reasonable alternative to carbapenems for the management of ESBL-producing pyelonephritis and may mitigate the risk of emergence of carbapenem-resistant organisms, compared with carbapenem therapy.<br />
DOI: 10.1093/cid/ciz1205 PMCID: PMC7643734 PMID: 31859352 [Indexed for MEDLINE]<br />
<br />
[5]. Lancet Infect Dis. 2019 Dec;19(12):1299-1311. doi: 10.1016/S1473-3099(19)30403-7. Epub 2019 Sep 25.<br />
Ceftolozane-tazobactam versus meropenem for treatment of nosocomial pneumonia (ASPECT-NP): a randomised, controlled, double-blind, phase 3, non-inferiority trial.<br />
Kollef MH(1), Nováček M(2), Kivistik Ü(3), Réa-Neto Á(4), Shime N(5), Martin-Loeches I(6), Timsit JF(7), Wunderink RG(8), Bruno CJ(9), Huntington JA(9), Lin G(9), Yu B(9), Butterton JR(9), Rhee EG(10).<br />
Author information: (1)Washington University School of Medicine, St Louis, MO, USA. (2)General Hospital of Kolin, Kolin, Czech Republic. (3)North Estonia Medical Centre, Tallinn, Estonia. (4)Universidade Federal do Paraná, Curitiba, Brazil. (5)Hiroshima University, Hiroshima, Japan. (6)St James's Hospital, Dublin, Ireland; Universitat de Barcelona, Instituto de Investigaciones Biomédicas August Pi i Sunyer, Centro de Investigación Biomédica en Red Enfermedades Respiratorias, Barcelona, Spain. (7)Université Paris Diderot, Paris, France. (8)Northwestern University Feinberg School of Medicine, Chicago, IL, USA. (9)Merck & Co, Kenilworth, NJ, USA. (10)Merck & Co, Kenilworth, NJ, USA. Electronic address: [email protected].<br />
Comment in Lancet Infect Dis. 2019 Dec;19(12):1266-1267. Lancet Infect Dis. 2020 Jan;20(1):20-21. Lancet Infect Dis. 2020 Jan;20(1):20.<br />
BACKGROUND: Nosocomial pneumonia due to antimicrobial-resistant pathogens is associated with high mortality. We assessed the efficacy and safety of the combination antibacterial drug ceftolozane-tazobactam versus meropenem for treatment of Gram-negative nosocomial pneumonia. METHODS: We conducted a randomised, controlled, double-blind, non-inferiority trial at 263 hospitals in 34 countries. Eligible patients were aged 18 years or older, were undergoing mechanical ventilation, and had nosocomial pneumonia (either ventilator-associated pneumonia or ventilated hospital-acquired pneumonia). Patients were randomly assigned (1:1) with block randomisation (block size four), stratified by type of nosocomial pneumonia and age (<65 years vs ≥65 years), to receive either 3 g ceftolozane-tazobactam or 1 g meropenem intravenously every 8 h for 8-14 days. The primary endpoint was 28-day all-cause mortality (at a 10% non-inferiority margin). The key secondary endpoint was clinical response at the test-of-cure visit (7-14 days after the end of therapy; 12·5% non-inferiority margin). Both endpoints were assessed in the intention-to-treat population. Investigators, study staff, patients, and patients' representatives were masked to treatment assignment. Safety was assessed in all randomly assigned patients who received study treatment. This trial was registered with ClinicalTrials.gov, NCT02070757. FINDINGS: Between Jan 16, 2015, and April 27, 2018, 726 patients were enrolled and randomly assigned, 362 to the ceftolozane-tazobactam group and 364 to the meropenem group. Overall, 519 (71%) patients had ventilator-associated pneumonia, 239 (33%) had Acute Physiology and Chronic Health Evaluation II scores of at least 20, and 668 (92%) were in the intensive care unit. At 28 days, 87 (24·0%) patients in the ceftolozane-tazobactam group and 92 (25·3%) in the meropenem group had died (weighted treatment difference 1·1% [95% CI -5·1 to 7·4]). At the test-of-cure visit 197 (54%) patients in the ceftolozane-tazobactam group and 194 (53%) in the meropenem group were clinically cured (weighted treatment difference 1·1% [95% CI -6·2 to 8·3]). Ceftolozane-tazobactam was thus non-inferior to meropenem in terms of both 28-day all-cause mortality and clinical cure at test of cure. Treatment-related adverse events occurred in 38 (11%) of 361 patients in the ceftolozane-tazobactam group and 27 (8%) of 359 in the meropenem group. Eight (2%) patients in the ceftolozane-tazobactam group and two (1%) in the meropenem group had serious treatment-related adverse events. There were no treatment-related deaths. INTERPRETATION: High-dose ceftolozane-tazobactam is an efficacious and well tolerated treatment for Gram-negative nosocomial pneumonia in mechanically ventilated patients, a high-risk, critically ill population. FUNDING: Merck & Co.<br />
DOI: 10.1016/S1473-3099(19)30403-7 PMID: 31563344 [Indexed for MEDLINE]
|