| Reference | [1]. N Engl J Med. 2019 Oct 31;381(18):1728-1740. doi: 10.1056/NEJMoa1902688.<br />
Gilteritinib or Chemotherapy for Relapsed or Refractory FLT3-Mutated AML.<br />
Perl AE(1), Martinelli G(1), Cortes JE(1), Neubauer A(1), Berman E(1), Paolini S(1), Montesinos P(1), Baer MR(1), Larson RA(1), Ustun C(1), Fabbiano F(1), Erba HP(1), Di Stasi A(1), Stuart R(1), Olin R(1), Kasner M(1), Ciceri F(1), Chou WC(1), Podoltsev N(1), Recher C(1), Yokoyama H(1), Hosono N(1), Yoon SS(1), Lee JH(1), Pardee T(1), Fathi AT(1), Liu C(1), Hasabou N(1), Liu X(1), Bahceci E(1), Levis MJ(1).<br />
Author information: (1)From the Abramson Cancer Center, University of Pennsylvania (A.E.P.), and Thomas Jefferson University (M.K.) – both in Philadelphia; Istituto Scientifico Romagnolo per lo Studio e la Cura dei Tumori, Istituto Di Ricovero e Cura a Carattere Scientifico (IRCCS), Meldola (G.M.), L. and A. Seràgnoli Institute of Hematology, Bologna University Medical School, Bologna (S.P.), Ospedali Riuniti Villa Sofia-Cervello, Palermo (F.F.), and IRCCS San Raffaele Scientific Institute, Milan (F.C.) – all in Italy; University of Texas M.D. Anderson Cancer Center, Houston (J.E.C.); Universitätsklinikum Giessen und Marburg, Marburg, Germany (A.N.); Memorial Sloan Kettering Cancer Center, New York (E. Berman); Hospital Universitari i Politècnic La Fe, Valencia, and Centro de Investigación Biomédica en Red Cáncer (CIBERONC), Instituto Carlos III, Madrid – both in Spain (P.M.); University of Maryland Greenebaum Comprehensive Cancer Center (M.R.B.) and Sidney Kimmel Comprehensive Cancer Center, Johns Hopkins University (M.J.L.) – both in Baltimore; University of Chicago, Chicago (R.A.L.), and Astellas Pharma, Northbrook (C.L., N. Hasabou, X.L., E. Bahceci) – both in Illinois; University of Minnesota, Minneapolis (C.U.); University of Alabama at Birmingham, Birmingham (H.P.E., A.D.S.); Hollings Cancer Center, Medical University of South Carolina, Charleston (R.S.); University of California, San Francisco, San Francisco (R.O.); National Taiwan University, Taipei City, Taiwan (W.-C.C.); Yale University School of Medicine, New Haven, CT (N.P.); Centre Hospitalier Universitaire de Toulouse, Institut Universitaire du Cancer de Toulouse Oncopole, Université Toulouse III Paul Sabatier, Toulouse, France (C.R.); Sendai Medical Center, National Hospital Organization, Sendai (H.Y.), and University of Fukui, Fukui (N. Hosono) – both in Japan; Seoul National University (S.-S.Y.) and Asan Medical Center, University of Ulsan College of Medicine (J.-H.L.) – both in Seoul, South Korea; Wake Forest Baptist Medical Center, Winston-Salem, NC (T.P.); and Massachusetts General Hospital, Harvard Medical School, Boston (A.T.F.).<br />
Comment in Nat Rev Clin Oncol. 2020 Feb;17(2):69.<br />
BACKGROUND: Patients with relapsed or refractory acute myeloid leukemia (AML) with mutations in the FMS-like tyrosine kinase 3 gene (FLT3) infrequently have a response to salvage chemotherapy. Gilteritinib is an oral, potent, selective FLT3 inhibitor with single-agent activity in relapsed or refractory FLT3-mutated AML. METHODS: In a phase 3 trial, we randomly assigned adults with relapsed or refractory FLT3-mutated AML in a 2:1 ratio to receive either gilteritinib (at a dose of 120 mg per day) or salvage chemotherapy. The two primary end points were overall survival and the percentage of patients who had complete remission with full or partial hematologic recovery. Secondary end points included event-free survival (freedom from treatment failure [i.e., relapse or lack of remission] or death) and the percentage of patients who had complete remission. RESULTS: Of 371 eligible patients, 247 were randomly assigned to the gilteritinib group and 124 to the salvage chemotherapy group. The median overall survival in the gilteritinib group was significantly longer than that in the chemotherapy group (9.3 months vs. 5.6 months; hazard ratio for death, 0.64; 95% confidence interval [CI], 0.49 to 0.83; P<0.001). The median event-free survival was 2.8 months in the gilteritinib group and 0.7 months in the chemotherapy group (hazard ratio for treatment failure or death, 0.79; 95% CI, 0.58 to 1.09). The percentage of patients who had complete remission with full or partial hematologic recovery was 34.0% in the gilteritinib group and 15.3% in the chemotherapy group (risk difference, 18.6 percentage points; 95% CI, 9.8 to 27.4); the percentages with complete remission were 21.1% and 10.5%, respectively (risk difference, 10.6 percentage points; 95% CI, 2.8 to 18.4). In an analysis that was adjusted for therapy duration, adverse events of grade 3 or higher and serious adverse events occurred less frequently in the gilteritinib group than in the chemotherapy group; the most common adverse events of grade 3 or higher in the gilteritinib group were febrile neutropenia (45.9%), anemia (40.7%), and thrombocytopenia (22.8%). CONCLUSIONS: Gilteritinib resulted in significantly longer survival and higher percentages of patients with remission than salvage chemotherapy among patients with relapsed or refractory FLT3-mutated AML. (Funded by Astellas Pharma; ADMIRAL ClinicalTrials.gov number, NCT02421939.).<br />
DOI: 10.1056/NEJMoa1902688 PMID: 31665578 [Indexed for MEDLINE]<br />
<br />
[2]. Biomark Res. 2019 Sep 11;7:19. doi: 10.1186/s40364-019-0170-2. eCollection 2019.<br />
Gilteritinib: a novel FLT3 inhibitor for acute myeloid leukemia.<br />
Zhao J(1), Song Y(1), Liu D(1)(2).<br />
Author information: (1)1Department of Oncology, The first Affiliated Hospital of Zhengzhou University, Zhengzhou, 450052 China. (2)2Division of Hematology & Oncology, New York Medical College, Valhalla, NY 10595 USA.<br />
Erratum in Biomark Res. 2019 Oct 17;7:21.<br />
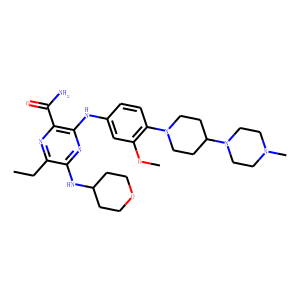
FMS-like tyrosine kinase 3- internal tandem duplication (FLT3-ITD) remains as one of the most frequently mutated genes in acute myeloid leukemia (AML), especially in those with normal cytogenetics. The FLT3-ITD and FLT3-TKD (tyrosine kinase domain) mutations are biomarkers for high risk AML and are associated with drug resistance and high risk of relapse. Multiple FLT3 inhibitors are in clinical development, including lestaurtinib, tandutinib, quizartinib, midostaurin, gilteritinib, and crenolanib. Midostaurin and gilteritinib have been approved by FDA for Flt3 mutated AML. Gilteritinib (ASP2215, Xospata) is a small molecule dual inhibitor of FLT3/AXL. The ADMIRAL study showed that longer overall survival and higher response rate are associated with gilteritinib in comparison with salvage chemotherapy for relapse /refractory (R/R) AML. These data from the ADMIRAL study may lead to the therapy paradigm shift and establish gilteritinib as the new standard therapy for R/R FLT3-mutated AML. Currently, multiple clinical trials are ongoing to evaluate the combination of gilteritinib with other agents and regimens. This study summarized clinical trials of gilteritinib for AML.<br />
DOI: 10.1186/s40364-019-0170-2 PMCID: PMC6737601 PMID: 31528345<br />
<br />
[3]. Drugs. 2019 Feb;79(3):331-339. doi: 10.1007/s40265-019-1062-3.<br />
Gilteritinib: First Global Approval.<br />
Dhillon S(1).<br />
Author information: (1)Springer, Private Bag 65901, Mairangi Bay, Auckland, 0754, New Zealand. [email protected].<br />
Gilteritinib (Xospata®) is an orally available small molecule receptor tyrosine kinase inhibitor developed by Astellas Pharma in collaboration with Kotobuki Pharmaceutical for the treatment of acute myeloid leukaemia (AML) harbouring FMS-like tyrosine kinase 3 (FLT3) mutations. Gilteritinib inhibits FLT3 (STK1 or FLK2), AXL (UFO or JTK11) and anaplastic lymphoma kinase (ALK or CD246). Gilteritinib inhibits FLT3 signalling in cells expressing FLT3 internal tandem duplication (ITD), tyrosine kinase domain mutation FLT3-D835Y and the double mutant FLT3-ITD-D835Y, thereby inducing apoptosis. Gilteritinib also binds to and inhibits the wild-type and mutated forms of ALK, resulting in reduced tumour cell proliferation in cancer cell types that overexpress the mutation. Gilteritinib is approved in Japan for the treatment of relapsed or refractory AML with FLT3 mutation. Recently, it was also approved in the USA for the treatment of adult patients who have relapsed or refractory AML with a FLT3 mutation, as detected by an FDA-approved test. Clinical development of gilteritinib is underway in several countries worldwide. Development for non-small cell lung cancer and solid tumours has been discontinued.<br />
DOI: 10.1007/s40265-019-1062-3 PMID: 30721452 [Indexed for MEDLINE]<br />
<br />
[4]. Clin Pharmacokinet. 2020 Oct;59(10):1273-1290. doi: 10.1007/s40262-020-00888-w.<br />
Pharmacokinetic Profile of Gilteritinib: A Novel FLT-3 Tyrosine Kinase Inhibitor.<br />
James AJ(1), Smith CC(2), Litzow M(3), Perl AE(4), Altman JK(5), Shepard D(6), Kadokura T(7), Souda K(7), Patton M(8), Lu Z(8), Liu C(8), Moy S(8), Levis MJ(9), Bahceci E(8).<br />
Author information: (1)Astellas Pharma US, Inc., 1 Astellas Way, Northbrook, IL, 60062, USA. [email protected]. (2)University of California San Francisco, San Francisco, CA, USA. (3)Mayo Clinic, Rochester, NY, USA. (4)University of Pennsylvania-Abramson Comprehensive Cancer Center, Philadelphia, PA, USA. (5)Robert H. Lurie Comprehensive Cancer Center of Northwestern University, Chicago, IL, USA. (6)Cleveland Clinic, Cleveland, OH, USA. (7)Astellas Pharma, Inc., Tokyo, Japan. (8)Astellas Pharma US, Inc., 1 Astellas Way, Northbrook, IL, 60062, USA. (9)John Hopkins University, Baltimore, MD, USA.<br />
Erratum in Clin Pharmacokinet. 2021 Jul 23;:<br />
BACKGROUND AND OBJECTIVE: Gilteritinib is a novel, highly selective tyrosine kinase inhibitor approved in the USA, Canada, Europe, Brazil, Korea, and Japan for the treatment of FLT3 mutation-positive acute myeloid leukemia. This article describes the clinical pharmacokinetic profile of gilteritinib. METHODS: The pharmacokinetic profile of gilteritinib was assessed from five clinical studies. RESULTS: Dose-proportional pharmacokinetics was observed following once-daily gilteritinib administration (dose range 20-450 mg). Median maximum concentration was reached 2-6 h following single and repeat dosing of gilteritinib; mean elimination half-life was 113 h. Elimination was primarily via feces. Exposure to gilteritinib was comparable under fasted and fed conditions. Gilteritinib is primarily metabolized via cytochrome P450 (CYP) 3A4; coadministration of gilteritinib with itraconazole (a strong P-glycoprotein inhibitor and CYP3A4 inhibitor) or rifampicin (a strong P-glycoprotein inducer and CYP3A inducer) significantly affected the gilteritinib pharmacokinetic profile. No clinically relevant interactions were observed when gilteritinib was coadministered with midazolam (a CYP3A4 substrate) or cephalexin (a multidrug and toxin extrusion 1 substrate). Unbound gilteritinib exposure was similar between subjects with hepatic impairment and normal hepatic function. CONCLUSIONS: Gilteritinib exhibits a dose-proportional pharmacokinetic profile in healthy subjects and in patients with relapsed/refractory acute myeloid leukemia. Gilteritinib exposure is not significantly affected by food. Moderate-to-strong CYP3A inhibitors demonstrated a significant effect on gilteritinib exposure. Coadministration of gilteritinib with CYP3A4 or multidrug and toxin extrusion 1 substrates did not impact substrate concentrations. Unbound gilteritinib was comparable between subjects with hepatic impairment and normal hepatic function; dose adjustment is not warranted for patients with hepatic impairment. CLINICAL TRIAL REGISTRATION: NCT02014558, NCT02456883, NCT02571816.<br />
DOI: 10.1007/s40262-020-00888-w PMCID: PMC7550323 PMID: 32304015<br />
<br />
[5]. Blood Adv. 2020 Mar 24;4(6):1178-1191. doi: 10.1182/bloodadvances.2019000174.<br />
Gilteritinib: potent targeting of FLT3 mutations in AML.<br />
Levis M(1), Perl AE(2).<br />
Author information: (1)Sidney Kimmel Comprehensive Cancer Center, Johns Hopkins University, Baltimore, MD; and. (2)Abramson Cancer Center, University of Pennsylvania, Philadelphia, PA.<br />
Since the discovery of FMS-like tyrosine kinase-3 (FLT3)-activating mutations as genetic drivers in acute myeloid leukemia (AML), investigators have tried to develop tyrosine kinase inhibitors that could effectively target FLT3 and alter the disease trajectory. Giltertinib (formerly known as ASP2215) is a novel compound that entered the field late, but moved through the developmental process with remarkable speed. In many ways, this drug's rapid development was facilitated by the large body of knowledge gained over the years from efforts to develop other FLT3 inhibitors. Single-agent gilteritinib, a potent and selective oral FLT3 inhibitor, improved the survival of patients with relapsed or refractory FLT3-mutated AML compared with standard chemotherapy. This continues to validate the approach of targeting FLT3 itself and establishes a new backbone for testing combination regimens. This review will frame the preclinical and clinical development of gilteritinib in the context of the lessons learned from its predecessors.<br />
DOI: 10.1182/bloodadvances.2019000174 PMCID: PMC7094008 PMID: 32208491 [Indexed for MEDLINE]
|