α-Glucosidase Inhibitors in Diabetes and Its Complications
Introduction
Diabetes is a chronic metabolic disorder characterized by high blood glucose levels resulting from defects in insulin secretion, insulin action, or both. There are two main types of diabetes: type 1 diabetes, which results from the destruction of insulin-producing beta cells in the pancreas, and type 2 diabetes, which results from insulin resistance and impaired insulin secretion[1]. Diabetes can lead to a range of complications, including microvascular complications (such as retinopathy, nephropathy, and neuropathy) and macrovascular complications (such as cardiovascular disease)[2,3]. Glycemic control, or the regulation of blood glucose levels, is a critical aspect of diabetes management. High blood glucose levels over an extended period can lead to various complications, including damage to the blood vessels, nerves, and organs. Therefore, maintaining optimal glycemic control is essential to prevent or delay the development of diabetes complications. Glycemic control can be influenced by several factors, such as diet, physical activity, medications, and insulin therapy. To maintain optimal glycemic control, people with diabetes should regularly monitor their blood glucose levels and adjust their treatment plan accordingly. In addition, adopting a healthy lifestyle that includes a balanced diet, regular exercise, and weight management can enhance glycemic control in individuals with diabetes. Managing glycemic control is a critical aspect of diabetes management since it can prevent or delay the onset of complications associated with diabetes. It is essential for people with diabetes to collaborate with their healthcare team to keep track of their blood glucose levels, make necessary adjustments to their treatment plan, and adopt lifestyle modifications to optimize their glycemic control.
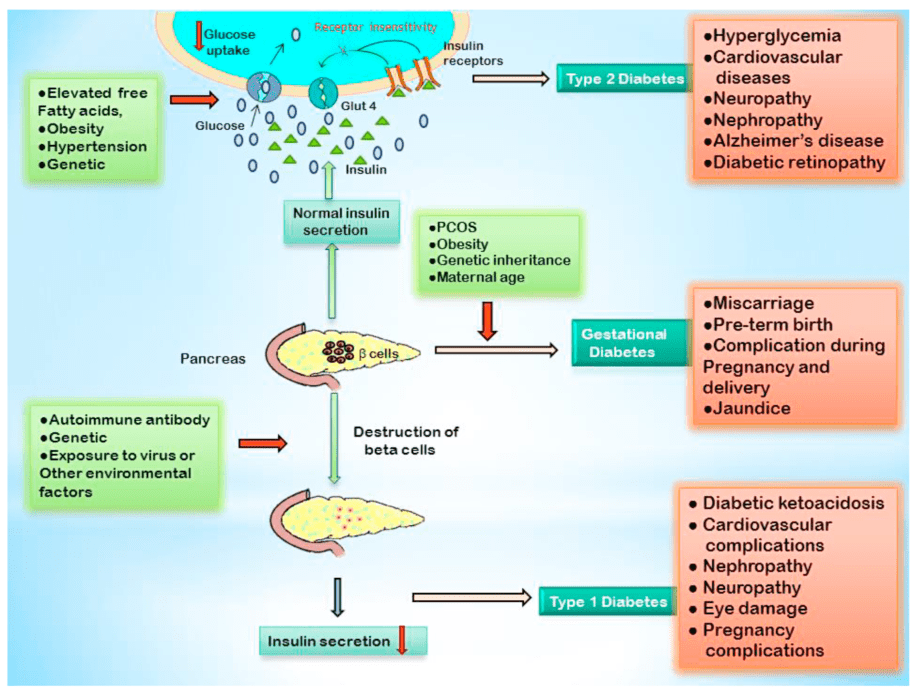
Figure 1 Schematic diagram of different types of diabetes, their cause, and consequences[4]
Role of α-glucosidase inhibitors in diabetes management
α-glucosidase inhibitors (AGIs) are a class of medications used in the management of diabetes[5]. They work by inhibiting the enzyme α-glucosidase, which is responsible for breaking down complex carbohydrates into simple sugars in the small intestine. By slowing down the digestion of carbohydrates, AGIs can help reduce the rise in blood glucose levels after meals, thereby improving glycemic control in individuals with diabetes. AGIs are particularly effective in controlling postprandial hyperglycemia, which is a significant contributor to overall glycemic control in individuals with diabetes. By reducing the spikes in blood glucose levels after meals, AGIs can help prevent or delay the development of diabetes complications, such as cardiovascular disease, neuropathy, and nephropathy. AGIs can be used as monotherapy or in combination with other antidiabetic medications, such as insulin, sulfonylureas, or metformin. They are generally well-tolerated, with gastrointestinal side effects such as flatulence, bloating, and diarrhea being the most common adverse effects. AGIs can also provide additional health benefits beyond glycemic control. They have been shown to have antioxidant, anti-inflammatory, and anti-obesity effects, potentially preventing or mitigating the development of other chronic diseases.
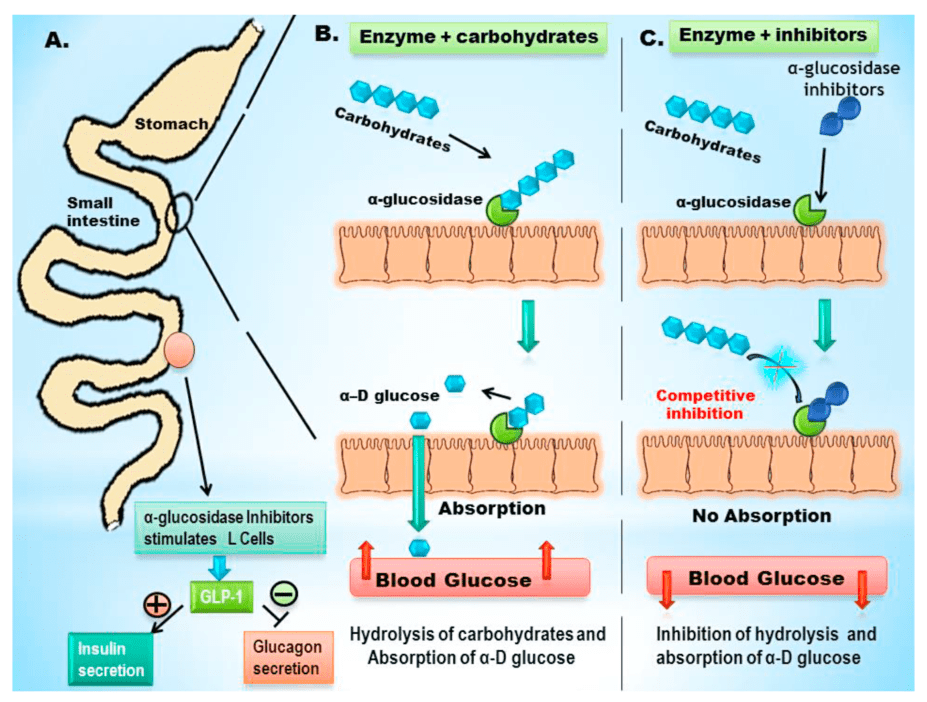
Figure 2 Role of α-glucosidase inhibitors in controlling postprandial hyperglycemia[4]
In summary, α-glucosidase inhibitors are an effective class of medications for the management of diabetes. They can improve glycemic control, particularly postprandial hyperglycemia, and potentially prevent or delay the development of diabetes complications. They are generally well-tolerated and can provide additional health benefits beyond glycemic control.
Mechanism of action of α-glucosidase inhibitors
AGIs are a medication class utilized in diabetes management that functions by inhibiting the enzyme α-glucosidase. This enzyme is responsible for breaking down complex carbohydrates into simple sugars in the small intestine. AGIs slow down carbohydrate digestion, thereby lowering the rise in blood glucose levels after meals and improving glycemic control in people with diabetes. The mechanism of action of AGIs involves several processes, including the inhibition of α-glucosidase enzyme activity, delayed glucose absorption, and reduced postprandial glucose levels.
Inhibition of α-glucosidase enzyme activity:
AGIs function by inhibiting the activity of the α-glucosidase enzyme in the small intestine, which breaks down complex carbohydrates into simple sugars for absorption into the bloodstream. The inhibition of this enzyme by AGIs results in a slower carbohydrate digestion process, leading to reduced glucose absorption into the bloodstream. Consequently, postprandial glucose levels decrease, thereby improving glycemic control in individuals with diabetes.
Delayed glucose absorption:
AGIs also work by delaying glucose absorption in the small intestine. This is because glucose absorption from the small intestine depends on the breakdown of carbohydrates by the α-glucosidase enzyme. By inhibiting the activity of this enzyme, AGIs delay the breakdown of carbohydrates and, subsequently, the absorption of glucose. This delay in glucose absorption can help reduce the spikes in blood glucose levels that occur after meals, thereby improving glycemic control in individuals with diabetes.
Reduction of postprandial glucose levels:
One of the main benefits of AGIs is their ability to reduce postprandial glucose levels. This is because the rise in blood glucose levels after meals is primarily due to the absorption of glucose from the small intestine. By inhibiting the α-glucosidase enzyme and delaying glucose absorption, AGIs can help reduce the rise in blood glucose levels after meals, leading to improved glycemic control in individuals with diabetes.
In summary, the mechanism of action of α-glucosidase inhibitors involves the inhibition of the α-glucosidase enzyme, delayed glucose absorption, and reduction of postprandial glucose levels. By slowing down the digestion of carbohydrates, AGIs can help reduce the spikes in blood glucose levels that occur after meals, leading to improved glycemic control in individuals with diabetes. AGIs are an effective class of medications for the management of diabetes and are generally well-tolerated, with gastrointestinal side effects being the most common adverse effects.
Bioactive α-glucosidase inhibitors
Numerous papers offer an extensive overview of bioactive α-glucosidase inhibitors that have been studied for their potential use in the management of diabetes and its complications. These inhibitors can be derived from various sources, including plants, microbes, and synthetic compounds.
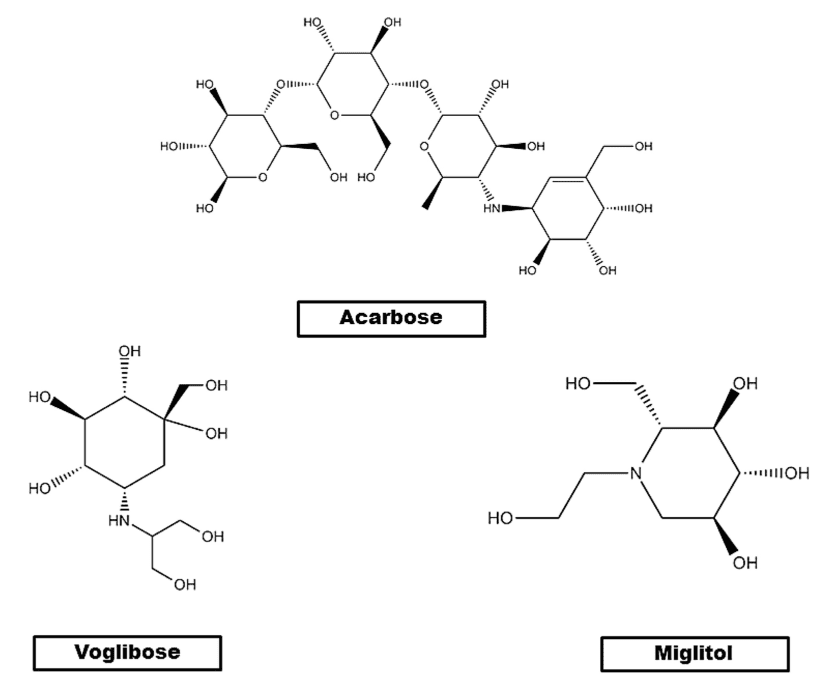
Figure 3 Chemical structures of commercially available α-glucosidase inhibitors.
Plant-derived α-glucosidase inhibitors are natural products that have shown α-glucosidase inhibitory activity and are potential candidates for treating diabetes. The paper discusses various plant-derived α-glucosidase inhibitors, such as polyphenols (e.g., EGCG from green tea, resveratrol from grapes and red wine, and quercetin from onions and apples), flavonoids (e.g., hesperidin from citrus fruits and rutin from buckwheat), and alkaloids (e.g., berberine from the Chinese herb Coptis chinensis).
Microbial α-glucosidase inhibitors, such as feruloylated oligosaccharides and polysaccharides from mushrooms (e.g., Agaricus blazei and Phellinus linteus), have also been studied for their potential therapeutic use in managing diabetes.
Synthetic α-glucosidase inhibitors, such as acarbose and miglitol, have been developed and used for years in diabetes management. They work by inhibiting the α-glucosidase enzyme in the small intestine, leading to delayed absorption of glucose and lower postprandial glucose levels.
Overall, bioactive α-glucosidase inhibitors have shown potential as therapeutic agents in diabetes management, and they can be derived from various sources. Plant-derived compounds have been extensively studied and have shown promising results in clinical and preclinical studies. Microbial-derived compounds and synthetic compounds also have potential as therapeutic agents, but further research is needed to fully understand their mechanism of action and potential clinical applications.
Pharmacological activities of α-glucosidase inhibitors
This paper discusses the pharmacological activities of α-glucosidase inhibitors beyond their antidiabetic activity. Here are some of the pharmacological activities of α-glucosidase inhibitors:
Antidiabetic activity:
The primary pharmacological activity of α-glucosidase inhibitors is their antidiabetic activity. By inhibiting α-glucosidase enzyme activity, these inhibitors delay glucose absorption and reduce postprandial glucose levels, which can help manage diabetes. Studies have shown that α-glucosidase inhibitors can improve glycemic control and reduce the risk of developing diabetic complications, such as diabetic retinopathy, neuropathy, and nephropathy.
Antioxidant activity:
Oxidative stress is a major contributor to the development of diabetic complications. α-glucosidase inhibitors have been found to possess antioxidant activity, which can help reduce oxidative stress and prevent the development of diabetic complications. Examples of plant-derived α-glucosidase inhibitors with antioxidant activity discussed in the paper include epigallocatechin gallate (EGCG) from green tea, resveratrol from grapes and red wine, and quercetin from onions and apples.
Anti-inflammatory activity:
Inflammation is another important contributor to the development of diabetic complications. α-glucosidase inhibitors have been found to possess anti-inflammatory activity, which can help reduce inflammation and prevent the development of diabetic complications. Examples of plant-derived α-glucosidase inhibitors with anti-inflammatory activity discussed in the paper include curcumin from turmeric and baicalin from Scutellaria baicalensis.
Anti-obesity activity:
Obesity is a major risk factor for the development of diabetes and its complications. α-glucosidase inhibitors have been found to possess anti-obesity activity, which can help prevent the development of diabetes and its complications. Studies have shown that α-glucosidase inhibitors can reduce body weight and improve lipid metabolism in animal models of obesity. Examples of plant-derived α-glucosidase inhibitors with anti-obesity activity discussed in the paper include quercetin from onions and apples and berberine from the Chinese herb Coptis chinensis.
Overall, α-glucosidase inhibitors have been found to possess a range of pharmacological activities beyond their antidiabetic activity. These inhibitors can possess antioxidant, anti-inflammatory, and anti-obesity activity, which can help prevent the development of diabetic complications. Plant-derived α-glucosidase inhibitors have been extensively studied and have shown promising results in preclinical and clinical studies. However, further research is needed to fully understand the mechanisms of action and potential clinical applications of microbial-derived and synthetic α-glucosidase inhibitors. Further research in this field may lead to the development of new therapies for the management of diabetes and its complications.
Potential benefits of α-glucosidase inhibitors in diabetic complications
Here are some of the potential benefits of α-glucosidase inhibitors in managing diabetic complications:
Nephropathy:
Diabetic nephropathy is progressive renal damage and a common complication of diabetes. α-glucosidase inhibitors have renoprotective effects that can prevent the development of diabetic nephropathy. Studies suggest that α-glucosidase inhibitors can decrease urinary protein excretion, prevent glomerular hypertrophy and mesangial expansion, and improve renal function in animal models of diabetes. Plant-derived α-glucosidase inhibitors, such as quercetin and EGCG, have shown promising results in preclinical studies and may be potential therapeutic agents for managing diabetic nephropathy.
Retinopathy:
Diabetic retinopathy is progressive damage to the retina and another common complication of diabetes. α-glucosidase inhibitors have antiangiogenic and antioxidative effects that can prevent the development of diabetic retinopathy. Studies suggest that α-glucosidase inhibitors can reduce retinal vascular permeability, prevent capillary degeneration, and improve visual function in animal models of diabetes. Plant-derived α-glucosidase inhibitors, such as EGCG and resveratrol, have shown promising results in preclinical studies and may be potential therapeutic agents for managing diabetic retinopathy.
Neuropathy:
Diabetic neuropathy is a common complication of diabetes and is characterized by progressive damage to the nerves. α-glucosidase inhibitors have been found to possess neuroprotective effects and can prevent the development of diabetic neuropathy. Studies have shown that α-glucosidase inhibitors can improve nerve conduction velocity, prevent nerve fiber loss, and reduce oxidative stress in animal models of diabetes. Plant-derived α-glucosidase inhibitors, such as EGCG and baicalin, have shown promising results in preclinical studies and may be potential therapeutic agents for the management of diabetic neuropathy.
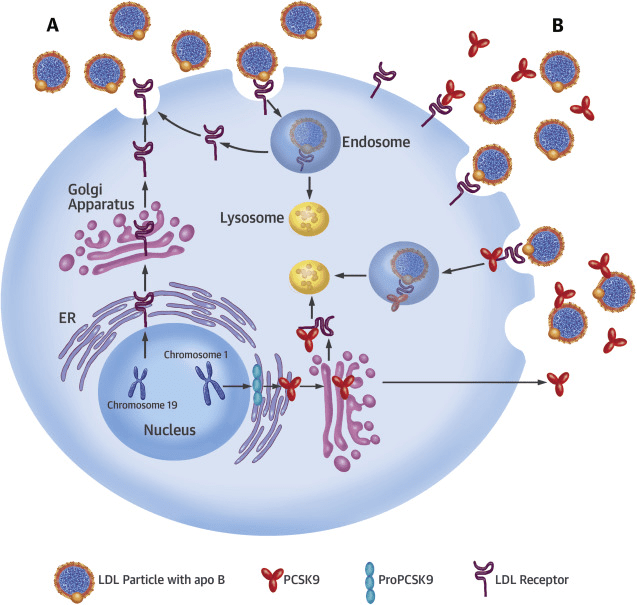
Cardiovascular complications:
Cardiovascular complications are a major cause of morbidity and mortality in diabetes. α-glucosidase inhibitors have been found to possess cardioprotective effects and can prevent the development of cardiovascular complications. Studies have shown that α-glucosidase inhibitors can improve endothelial function, reduce oxidative stress and inflammation, and prevent atherosclerosis in animal models of diabetes. Clinical studies have also shown that α-glucosidase inhibitors can reduce the risk of cardiovascular events in patients with diabetes. Plant-derived α-glucosidase inhibitors, such as EGCG and quercetin, have shown promising results in preclinical studies and may be potential therapeutic agents for the management of cardiovascular complications in diabetes.
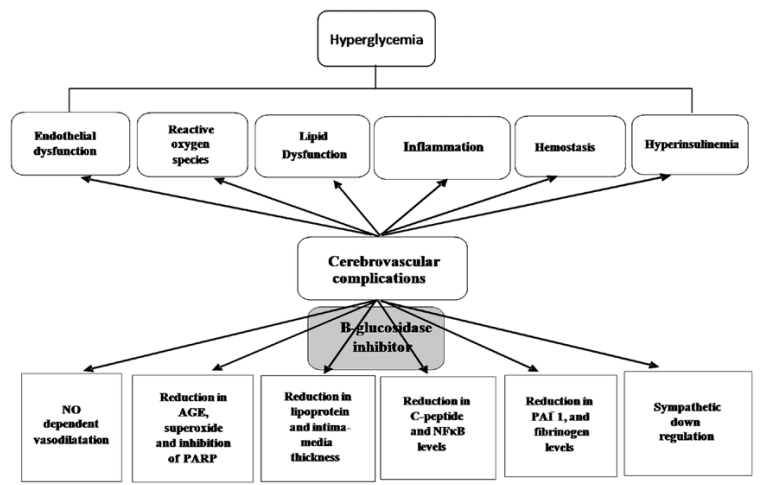
Figure 4 Potential mechanisms of α-glucosidase inhibitor in cerebrovascular protection.[6]
The potential benefits of α-glucosidase inhibitors in managing diabetic complications, such as nephropathy, retinopathy, neuropathy, and cardiovascular issues, have been widely reported. Plant-derived inhibitors have shown promise in both preclinical and clinical studies and may be a viable therapeutic option for treating diabetic complications. Nonetheless, further research is required to completely comprehend the mechanisms and possible clinical applications of microbial-derived and synthetic α-glucosidase inhibitors. Advancements in this field could result in the development of novel therapies for diabetes management and its complications.
Future directions for research on α-glucosidase inhibitors and their use in diabetes management
The following are some of the potential areas for future research that have been highlighted in this paper concerning α-glucosidase inhibitors and their use in diabetes management:
New α-glucosidase inhibitors development: Although natural sources of α-glucosidase inhibitors have shown promise, it is necessary to create new α-glucosidase inhibitors with improved pharmacological properties and fewer side effects.
Clinical trials: Although some clinical trials have demonstrated the efficacy of α-glucosidase inhibitors in diabetes management, further research is required to fully comprehend their clinical applications, potential benefits, and long-term safety.
Combination therapy: α-glucosidase inhibitors can be used in combination with other antidiabetic drugs, such as metformin and sulfonylureas, to improve glycemic control and reduce the risk of diabetic complications. Further studies are needed to explore the potential benefits and safety of combination therapy.
Mechanisms of action: Further research is needed to fully understand the mechanisms of action of α-glucosidase inhibitors and their potential effects on various pathways involved in the development of diabetic complications.
Personalized medicine: Further research is needed to explore the potential of personalized medicine in diabetes management, including the use of α-glucosidase inhibitors based on individual patient characteristics and disease severity.
Overall, further research in these areas may lead to the development of new and improved therapies for the management of diabetes and its complications.
Reference
- Cho, N. H., Shaw, J. E., Karuranga, S., Huang, Y., da Rocha Fernandes, J. D., Ohlrogge, A. W., & Malanda, B. I. D. F. (2018). IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes research and clinical practice, 138, 271-281.
- Esser, N., Paquot, N., & Scheen, A. J. (2015). Anti-inflammatory agents to treat or prevent type 2 diabetes, metabolic syndrome and cardiovascular disease. Expert opinion on investigational drugs, 24(3), 283-307.
- Rashid, K., Chowdhury, S., Ghosh, S., & Sil, P. C. (2017). Curcumin attenuates oxidative stress induced NFκB mediated inflammation and endoplasmic reticulum dependent apoptosis of splenocytes in diabetes. Biochemical pharmacology, 143, 140-155.
- Hossain, U., Das, A. K., Ghosh, S., & Sil, P. C. (2020). An overview on the role of bioactive α-glucosidase inhibitors in ameliorating diabetic complications. Food and chemical toxicology, 145, 111738.
- Kumar, S., Narwal, S., Kumar, V., & Prakash, O. (2011). [alpha]-glucosidase inhibitors from plants: A natural approach to treat diabetes. Pharmacognosy reviews, 5(9), 19.
- Patel, S. S. (2016). Cerebrovascular complications of diabetes: alpha glucosidase inhibitor as potential therapy. Hormone and Metabolic Research, 48(02), 83-91.