Understanding Fructose Malabsorption
Abstract
Fructose malabsorption (FM) is a prevalent gastrointestinal disorder characterized by the small intestine’s inability to properly absorb fructose, leading to symptoms such as bloating, cramps, and diarrhea. This condition is closely associated with irritable bowel syndrome (IBS) and can significantly impact the quality of life. FM can be caused by congenital enzyme deficiencies or secondary factors such as intestinal damage and infections. Diagnosis primarily involves the hydrogen breath test (HBT), although additional measures are often needed due to the nonspecific nature of symptoms. Effective management typically involves dietary modifications, notably a low-FODMAP diet, which restricts high-fructose foods. Enzymatic treatments like xylose isomerase offer promising alternatives for those who do not respond well to diet changes. Recent studies on fructose isotopes and transport proteins provide deeper insights into improving diagnosis and treatment. A comprehensive approach combining diet, enzymatic therapies, and alternative treatments can enhance the quality of life for individuals with FM. Further research is essential to refine these strategies and develop new interventions.
Introduction
Fructose malabsorption (FM) is a common yet often overlooked digestive disorder that impacts the ability of the small intestine to absorb fructose, a sugar found naturally in many foods and added to others. This condition can lead to a variety of gastrointestinal symptoms, including bloating, cramps, and diarrhea, which significantly affect the quality of life. Fructose malabsorption is particularly associated with conditions such as irritable bowel syndrome (IBS) and infantile colic, making its understanding crucial for effective health management.
The rise in FM cases parallels the increasing consumption of high fructose corn syrup (HFCS) and other fructose-rich foods in modern diets. This surge highlights the importance of recognizing and addressing FM in clinical practice and public health strategies. While primary causes of FM can be congenital, secondary causes such as intestinal damage, gastroenteritis, and medications are also significant contributors. Despite its prevalence, diagnosing FM remains challenging due to overlapping symptoms with other carbohydrate malabsorption disorders and the limitations of current diagnostic tools like the hydrogen breath test (HBT) (Benardout et al., 2021).
Effective management of FM primarily involves dietary modifications, particularly the low-FODMAP diet, which restricts foods high in fermentable oligo-, di-, monosaccharides, and polyols. This diet has been shown to alleviate symptoms in many patients, though adherence can be difficult and may require guidance from dietitians. Enzymatic treatments such as xylose isomerase, which converts fructose to glucose, offer promising alternatives. Additionally, understanding the role of transport proteins GLUT2 and GLUT5 in fructose absorption and the effect of fructose isotopes can further refine treatment strategies.
Continued research is essential to deepen our understanding of FM, improve diagnostic accuracy, and develop more effective treatments. This comprehensive approach will better equip healthcare providers to manage this condition and enhance the well-being of those affected.
What is Fructose Malabsorption?
Fructose malabsorption (FM) is a condition where the small intestine is unable to absorb fructose properly, leading to various gastrointestinal symptoms such as bloating, abdominal pain, cramps, and diarrhea. These symptoms arise due to the accumulation of fructose in the intestine, which increases osmotic pressure and draws water into the lumen, causing discomfort. FM is commonly associated with irritable bowel syndrome (IBS), a disorder characterized by recurrent abdominal pain and altered bowel habits. It is estimated that up to one-third of individuals with IBS may also suffer from FM.
The connection between FM and IBS highlights the importance of understanding this condition. IBS itself affects approximately 11% of the global population, with symptoms that significantly impact daily life and well-being. FM can be primary, caused by congenital issues such as enzyme deficiencies, or secondary, resulting from factors like intestinal damage, acute gastroenteritis, or conditions like Crohn’s disease and celiac disease.
One notable aspect of FM is its relationship with diet, particularly the consumption of high-fructose foods and beverages. The increased intake of high fructose corn syrup (HFCS), commonly found in soft drinks and processed foods, has been linked to a rise in FM cases. This dietary trend is especially prevalent among younger populations who consume large quantities of HFCS-rich products.
Despite its prevalence, FM often goes undiagnosed or is misdiagnosed due to its overlapping symptoms with other gastrointestinal disorders. Accurate diagnosis typically involves a hydrogen breath test (HBT), which measures hydrogen levels in the breath after fructose consumption. Elevated levels indicate malabsorption, although this test can sometimes yield false positives or negatives.
Causes and Diagnosis of Fructose Malabsorption
Fructose malabsorption (FM) can stem from both primary and secondary causes. Primary FM, also known as hereditary fructose intolerance, is a rare genetic disorder where the body lacks the enzyme aldolase B, necessary for the metabolism of fructose. This enzyme deficiency leads to the buildup of fructose-1-phosphate in the liver, kidneys, and small intestine, causing severe hypoglycemia and other metabolic complications. Secondary FM is more common and can result from various conditions that damage the intestinal lining, such as acute gastroenteritis, Crohn’s disease, celiac disease, and the prolonged use of certain medications like antibiotics.
Dietary habits significantly influence FM, particularly the consumption of foods high in fructose, such as fruits, honey, and foods sweetened with high fructose corn syrup (HFCS). The widespread use of HFCS in processed foods and beverages has led to an increase in FM cases, as this form of sugar is more readily absorbed than others and can overwhelm the small intestine’s capacity to process it. High intake of HFCS is especially prevalent among younger populations, contributing to the rise in FM diagnoses.
Diagnosing FM is challenging due to its nonspecific symptoms, which overlap with other gastrointestinal disorders like irritable bowel syndrome (IBS) and lactose intolerance. The hydrogen breath test (HBT) is the primary diagnostic tool used to identify FM. This test measures the amount of hydrogen in the breath after the ingestion of fructose. Elevated levels of hydrogen indicate that fructose has not been properly absorbed in the small intestine and has been fermented by bacteria in the colon, producing hydrogen gas as a byproduct. Despite its utility, the HBT can sometimes produce false positives or negatives, necessitating additional diagnostic measures and dietary assessments to confirm FM.
The Effect of Fructose Isotopes on Fructose Absorption
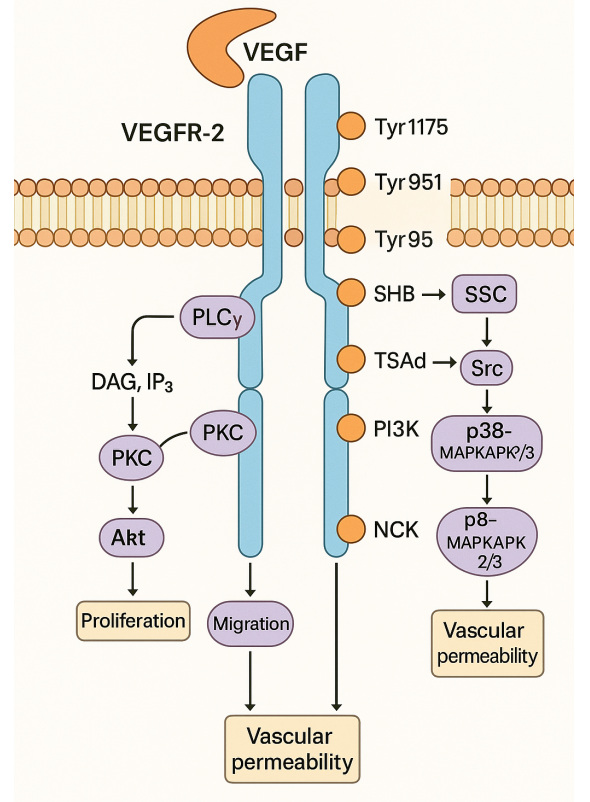
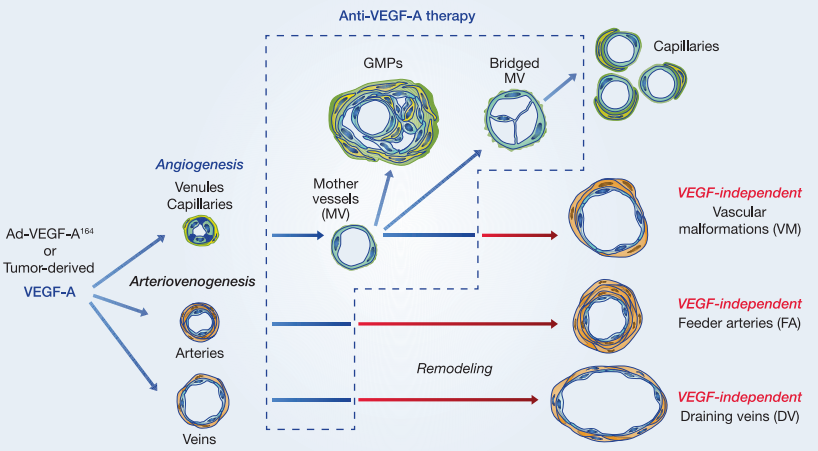
Fructose absorption in the small intestine involves several transport proteins and can be influenced by the chemical structure and isotopic forms of fructose. Fructose exists in various isomeric forms, including furanose and pyranose, which can affect absorption efficiency. The primary transporters involved in fructose absorption are GLUT2 and GLUT5. GLUT5 is mainly responsible for the initial uptake of fructose at the apical membrane of enterocytes, while GLUT2 facilitates the transfer of fructose from enterocytes into the bloodstream.
Recent studies have explored the impact of different fructose isotopes on absorption efficiency. Isotopes are variants of a particular chemical element that differ in neutron number. In the context of fructose, stable isotopes such as carbon-13 (13C) labeled fructose have been used in metabolic studies to gain deeper insights into the absorption kinetics and metabolic fate of fructose in the human body. 13C-labeled fructose (13C fructose) is particularly useful in tracing and measuring the absorption and metabolism of fructose without the risks associated with radioactive isotopes.
The structural form of fructose plays a critical role in its absorption. Fructose predominantly exists in its furanose form in solution but can also cyclize to form the pyranose ring structure. These structural variations influence how fructose interacts with its transporters. GLUT5, for instance, shows a higher affinity for the furanose form of fructose, which is the more common form found in nature. Studies using 13C fructose have shown that the efficiency of fructose absorption can vary depending on the form and concentration of fructose presented to the transporters.
These studies highlight the significant role of GLUT5 in selectively transporting fructose across the apical membrane of the small intestine. The low capacity but high specificity of GLUT5 means that when fructose is present in high concentrations, such as after consuming HFCS-rich foods, GLUT5 can become saturated. This saturation leads to incomplete absorption and the subsequent gastrointestinal symptoms associated with fructose malabsorption.
In addition to structural aspects, the interaction between fructose and other dietary sugars also affects its absorption. The presence of glucose enhances fructose absorption via the GLUT2 transporter. This co-transport mechanism underscores the complexity of fructose metabolism and the need for further research to optimize dietary recommendations for individuals with fructose malabsorption.
Understanding the nuances of fructose absorption, including the impact of isotopes and structural forms, can lead to better diagnostic and therapeutic strategies for managing fructose malabsorption. Further research is essential to fully elucidate these mechanisms and improve the quality of life for affected individuals.
Dietary Management
Effective dietary management is crucial for individuals with fructose malabsorption (FM) to alleviate symptoms and improve quality of life. One of the primary strategies is the adoption of a low-FODMAP diet, which involves reducing the intake of fermentable oligo-, di-, monosaccharides, and polyols. This diet has been shown to significantly reduce gastrointestinal symptoms in many patients with FM by limiting the consumption of foods that are poorly absorbed in the small intestine and subsequently fermented by gut bacteria.
The low-FODMAP diet emphasizes avoiding high-fructose foods, such as certain fruits (e.g., apples, pears, mangoes), honey, and high fructose corn syrup (HFCS)-laden products. Instead, individuals are encouraged to consume low-fructose alternatives like bananas, berries, citrus fruits, and glucose-based sweeteners. This substitution helps manage the symptoms by ensuring that fructose is adequately absorbed without overwhelming the transport capacity of GLUT5, the main transporter for fructose in the small intestine.

Adhering to a low-FODMAP diet can be challenging due to the prevalence of fructose in many processed foods and the need for careful meal planning. Therefore, it is often recommended that patients work with a dietitian specialized in FODMAP diets to ensure nutritional balance and proper adherence. Dietitians can provide personalized guidance, meal plans, and strategies to identify and avoid high-fructose foods, thus making the dietary transition smoother and more effective.
Additionally, understanding individual tolerance levels is important, as some people with FM may be able to tolerate small amounts of fructose without experiencing symptoms. This personalized approach to dietary management can help optimize the balance between symptom relief and dietary variety, enhancing the overall effectiveness of the treatment.
Treatment Options
Treating fructose malabsorption (FM) involves a combination of dietary modifications, enzymatic treatments, and alternative therapies to manage symptoms and improve overall digestive health. The primary approach is dietary intervention, specifically the low-FODMAP diet, which reduces the intake of fermentable carbohydrates that exacerbate symptoms. This diet has been effective for many patients, but it requires careful planning and guidance from dietitians to ensure nutritional balance and adherence.
In addition to dietary changes, enzymatic treatments such as xylose isomerase have shown promise in managing FM. Xylose isomerase converts fructose into glucose, which is more easily absorbed by the intestine. A study demonstrated that oral administration of xylose isomerase significantly reduced hydrogen production in breath tests, indicating improved fructose absorption, and alleviated gastrointestinal symptoms like abdominal pain and bloating. This enzymatic treatment offers an alternative for patients who struggle to adhere to strict dietary restrictions or who continue to experience symptoms despite dietary changes.
Another emerging treatment option is gut-directed hypnotherapy, which targets the gut-brain axis to alleviate gastrointestinal symptoms. This approach has shown similar efficacy to the low-FODMAP diet in reducing symptoms of irritable bowel syndrome (IBS) associated with FM. A randomized clinical trial found that hypnotherapy significantly improved symptoms without the dietary restrictions, providing a viable alternative for patients.
These treatment options highlight the importance of a multifaceted approach to managing FM. While dietary changes remain the cornerstone of treatment, enzymatic therapies.
Conclusion
Fructose malabsorption (FM) is a significant gastrointestinal condition that affects many individuals worldwide, often in conjunction with irritable bowel syndrome (IBS). The inability of the small intestine to properly absorb fructose leads to uncomfortable symptoms such as bloating, cramps, and diarrhea, which can severely impact the quality of life. Understanding the causes, diagnosis, and treatment options for FM is crucial for effective management and improved patient outcomes.
The primary causes of FM can be either congenital or secondary to other medical conditions like intestinal damage and infections. Diagnosing FM is challenging due to the nonspecific nature of its symptoms, which often overlap with other gastrointestinal disorders. The hydrogen breath test (HBT) remains a key diagnostic tool, although its limitations necessitate additional diagnostic measures and comprehensive dietary assessments.
Effective management of FM largely depends on dietary modifications, particularly the adoption of a low-FODMAP diet, which has proven effective in reducing symptoms for many patients. This diet involves avoiding foods high in fermentable carbohydrates, including certain fruits, sweeteners, and processed foods containing high fructose corn syrup (HFCS). Enzymatic treatments like xylose isomerase, which converts fructose to glucose, offer promising alternative therapies for those who find dietary changes insufficient.
Further research is essential to better understand the mechanisms of fructose absorption and to develop more accurate diagnostic tools and effective treatments. Studies on the role of fructose isotopes and transport proteins such as GLUT5 provide valuable insights into improving therapeutic strategies. A multifaceted approach that combines dietary management, enzymatic treatments, and alternative therapies like gut-directed hypnotherapy can significantly enhance the quality of life for individuals with FM.
In conclusion, while fructose malabsorption presents considerable challenges, ongoing research and comprehensive treatment strategies hold promise for better management and relief of symptoms, ultimately improving patient well-being.
References
- Benardout, M., Le Gresley, A., ElShaer, A., & Wren, S. P. (2021). Fructose malabsorption: Causes, diagnosis, and treatment. British Journal of Nutrition, 127, 481–489.
- Canavan, C., West, J., & Card, T. (2014). The epidemiology of irritable bowel syndrome. Clinical Epidemiology, 6, 71–80.
- Holtmann, G. J., Ford, A. C., & Talley, N. J. (2016). Pathophysiology of irritable bowel syndrome. The Lancet Gastroenterology & Hepatology, 1(2), 133–146.
- Di Nicolantonio, J. J., & Lucan, S. C. (2015). Is fructose malabsorption a cause of irritable bowel syndrome? Medical Hypotheses, 85(3), 295–297.
- Choi, Y. K., Kraft, N., Zimmerman, B., et al. (2008). Fructose intolerance in IBS and utility of fructose-restricted diet. Journal of Clinical Gastroenterology, 42(3), 233–238.
- Vos, M. B., Kimmons, J. E., Gillespie, C., Welsh, J., & Blanck, H. M. (2008). Dietary fructose consumption among US children and adults: The Third National Health and Nutrition Examination Survey. Medscape Journal of Medicine, 10(7), 160.
- Douard, V., & Ferraris, R. P. (2008). Regulation of the fructose transporter GLUT5 in health and disease. American Journal of Physiology-Endocrinology and Metabolism, 295(2), E227-E237.
- Ferraris, R. P. (2001). Dietary and developmental regulation of intestinal sugar transport. Biochemical Journal, 360(2), 265-276.
- Rumessen, J. J., & Gudmand-Høyer, E. (1998). Fructans of chicory: Intestinal transport and fermentation of different chain lengths and relation to fructose and sorbitol malabsorption. American Journal of Clinical Nutrition, 68(2), 357-364.
- Truswell, A. S., Seach, J. M., & Thorburn, A. W. (1988). Incomplete absorption of pure fructose in healthy subjects and the facilitating effect of glucose. American Journal of Clinical Nutrition, 48(6), 1424-1430.
- Halmos, E. P., Power, V. A., Shepherd, S. J., Gibson, P. R., & Muir, J. G. (2014). A diet low in FODMAPs reduces symptoms of irritable bowel syndrome. Gastroenterology, 146(1), 67-75.
- Nanayakkara, W. S., Skidmore, P. M., O’Brien, L., Wilkinson, T. J., & Gearry, R. B. (2016). Efficacy of the low FODMAP diet for treating irritable bowel syndrome: The evidence to date. Clinical and Experimental Gastroenterology, 9, 131-142.
- Shepherd, S. J., Parker, F. C., Muir, J. G., & Gibson, P. R. (2008). Dietary triggers of abdominal symptoms in patients with irritable bowel syndrome: Randomized placebo-controlled evidence. Clinical Gastroenterology and Hepatology, 6(7), 765-771.
- Komericki, P., Akkilic-Materna, M., Strimitzer, T., et al. (2012). Oral xylose isomerase decreases breath hydrogen excretion and improves gastrointestinal symptoms in fructose malabsorption: A double-blind, placebo-controlled study. Alimentary Pharmacology & Therapeutics, 36(10), 980-987.
- Lindfors, P., Unge, P., Arvidsson, P., et al. (2012). Effects of gut-directed hypnotherapy on IBS in different clinical settings—results from two randomized, controlled trials. The American Journal of Gastroenterology, 107(2), 276-285.