The Relationship Between Gut Microbiota and Cancer
Abstract
Since the beginning of the 21st century, significant breakthroughs have been made in cancer research, among which the association between gut microbiota and cancer has garnered increasing attention. A growing body of evidence suggests that gut microbiota can influence the host’s response to cancer therapy by modulating the immune system. This paper aims to review the relationship between gut microbiota and cancer, with a particular focus on its impact on immunotherapy efficacy. It summarizes recent research advances and explores future challenges and research directions.
Introduction
Cancer remains one of the leading threats to global public health. Traditionally, cancer treatment has focused on surgery, chemotherapy, radiotherapy, and targeted therapies. In recent years, as the relationship between the immune system and cancer has become better understood, immunotherapy has emerged as a major breakthrough in the oncology field.
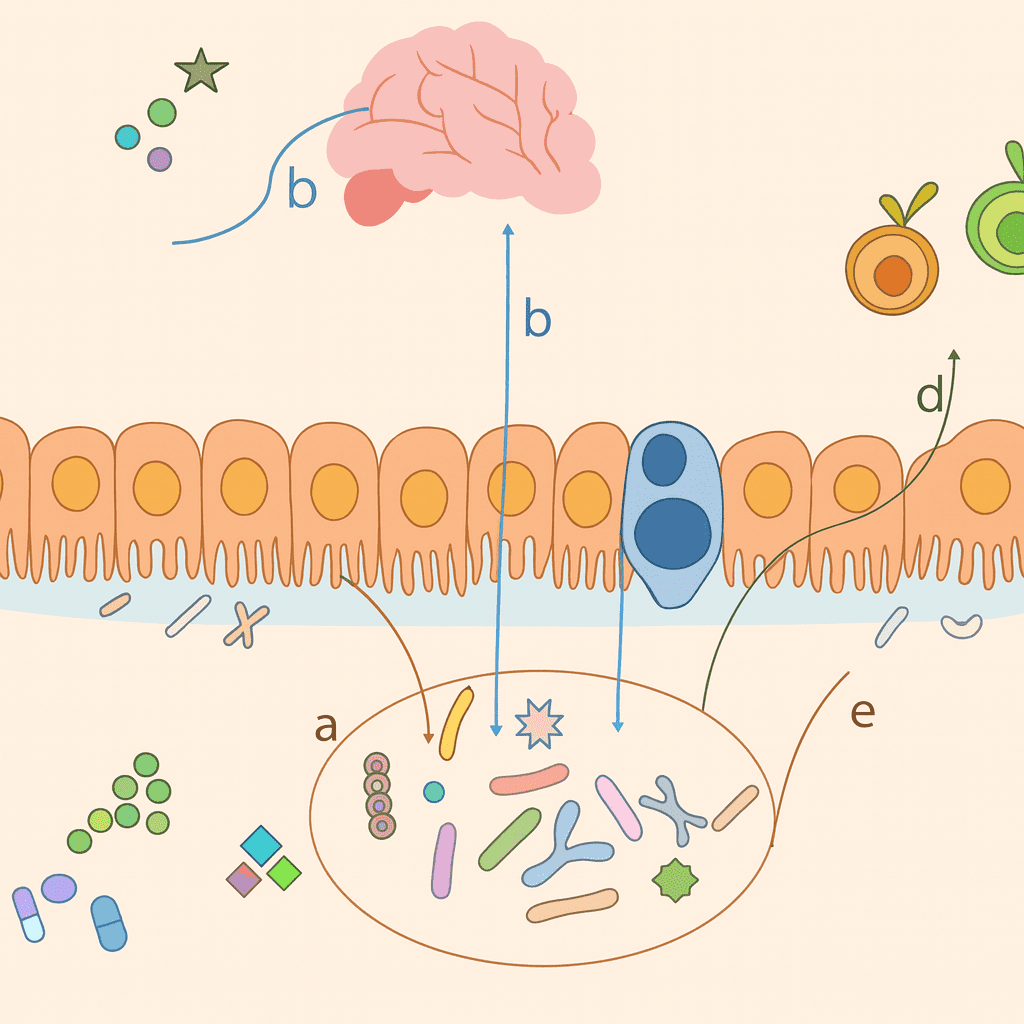
Meanwhile, increasing research has revealed that gut microbiota—a vast and complex microbial community residing in the human intestine—plays a crucial role in cancer initiation, progression, and treatment. Comprising trillions of bacteria, fungi, and viruses, gut microbiota forms a complex symbiotic relationship with the host and participates in various physiological processes, including digestion, metabolism, and immune regulation.
Understanding the interactions between gut microbiota and cancer is of great significance for developing more effective therapeutic strategies, improving treatment outcomes, and enhancing the quality of life for cancer patients.

Regulation of the Immune System by Gut Microbiota
Activation of Innate and Adaptive Immune Systems
The gut microbiota is a vital component of the human immune system, playing a key role in its development and functionality. A pioneering study in 2013 by Laurence Zitvogel and Giorgio Trinchieri’s team demonstrated that a complete gut microbiota is essential for initiating both innate and adaptive immune responses in the host, thereby enhancing the efficacy of three different anticancer therapies.
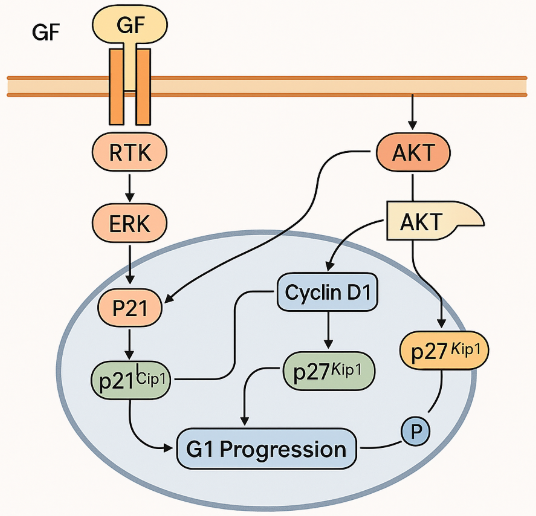
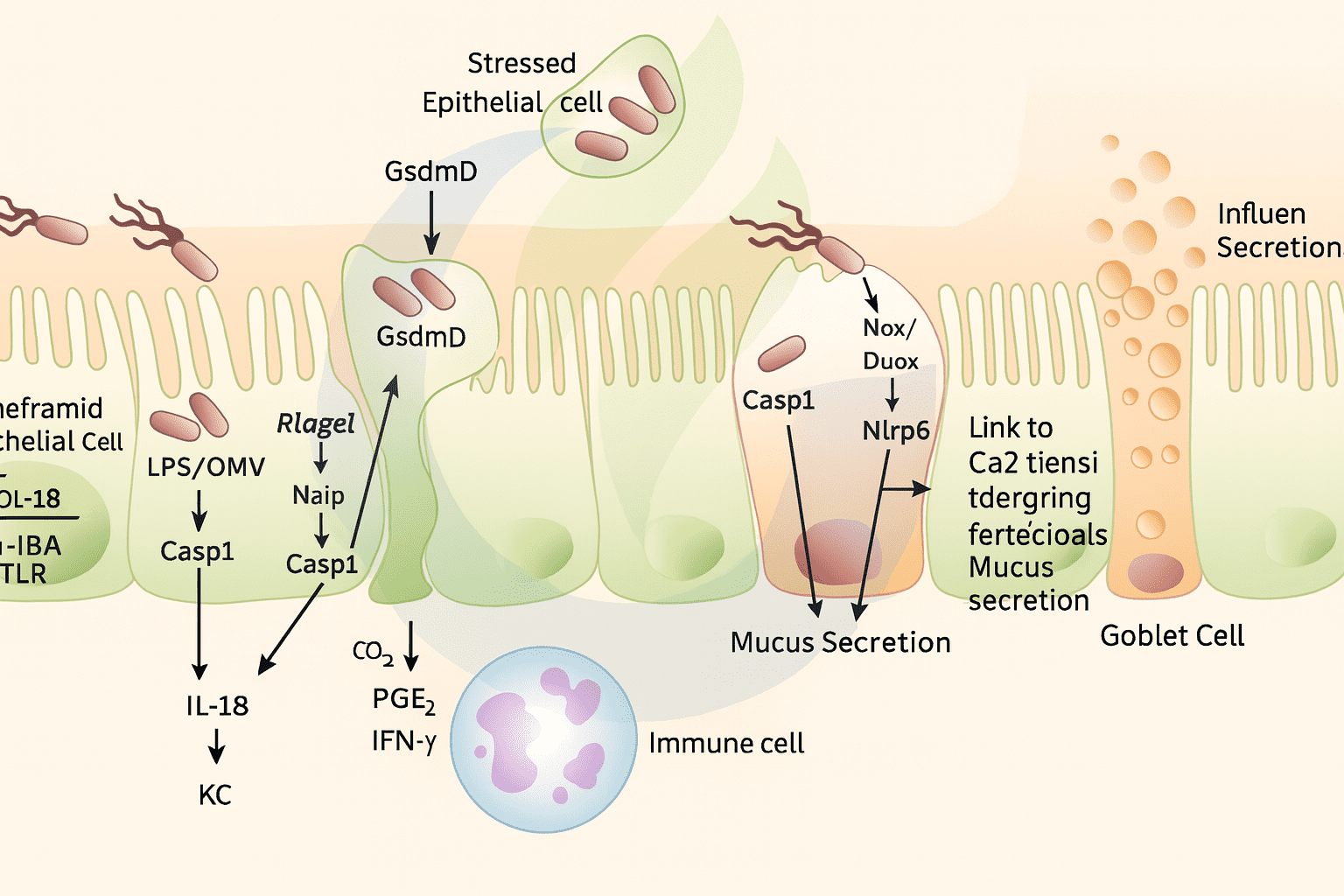
Innate immunity serves as the body’s first line of defense against pathogens. It involves the activation of immune cells such as macrophages and natural killer (NK) cells, and the initiation of inflammatory responses. Gut microbiota can interact with pattern recognition receptors on intestinal epithelial cells and immune cells to trigger signaling pathways that activate innate immune cells and promote the release of inflammatory mediators.
Adaptive immunity, on the other hand, is a specific defense mechanism involving T cells and B cells. Gut microbiota supports the development of gut-associated lymphoid tissue and promotes the differentiation and maturation of T and B cells, thereby enhancing the strength and specificity of adaptive immune responses.
Modulation of Immune Cell Function and Activity
Gut microbiota can also modulate the function and activity of immune cells, influencing the immune system’s response to cancer. For instance, certain microbial species can induce the production of regulatory T cells (Tregs), which suppress immune responses and play a crucial role in maintaining immune tolerance and preventing autoimmune diseases. However, in the tumor microenvironment, overactivation of Tregs may inhibit antitumor immune responses and promote tumor growth and metastasis.
Conversely, some gut microbes can activate effector T cells and natural killer cells, boosting their ability to eliminate tumor cells. Gut microbiota also influences macrophage polarization, shifting them from the tumor-promoting M2 phenotype to the tumor-fighting M1 phenotype, thus altering the immunological state of the tumor microenvironment.
Impact of Gut Microbiota on Cancer Therapy Response
Influence on Immunotherapy Efficacy
Immunotherapy has emerged as a prominent approach in cancer treatment in recent years, including immune checkpoint inhibitors (ICIs) and adoptive cell therapies.
An increasing number of studies have shown that the composition and functionality of gut microbiota are closely linked to the effectiveness of immunotherapy. In 2018, research led by Zitvogel, Gajeski, and Jennifer Wargo revealed that commensal gut bacteria influence the efficacy of anti-PD-1 immune checkpoint inhibitors in patients with melanoma and epithelial cancers. Specifically, the presence of certain beneficial bacteria in the gut enhances the immune system’s ability to recognize and destroy cancer cells, thus improving therapeutic outcomes. Conversely, dysbiosis or an overabundance of harmful bacteria may lead to immunotherapy resistance and reduced efficacy.
For example, beneficial species like Bifidobacterium spp. can activate dendritic cells and promote T cell activation and proliferation, thereby boosting antitumor immune responses. On the other hand, harmful bacteria such as Fusobacterium nucleatum are enriched in tumor tissues and associated with immunotherapy resistance in colorectal cancer patients, likely by impairing immune cell function and promoting tumor immune evasion.
Influence on Chemotherapy and Radiotherapy Outcomes
Beyond immunotherapy, gut microbiota also impacts the effectiveness of chemotherapy and radiotherapy.
While these treatments target tumor cells, they also harm normal tissues and cause side effects. Gut microbiota can alleviate these adverse effects by modulating immune responses and metabolic pathways, thereby improving patient tolerance. For instance, some studies have shown that gut microbes enhance the intestinal mucosal barrier, reducing mucosal damage caused by chemotherapy agents and lowering the incidence of gastrointestinal side effects such as diarrhea and nausea.
Moreover, gut microbiota can affect the metabolism and distribution of chemotherapy drugs, altering drug concentration and efficacy within tumor tissues.
Regarding radiotherapy, the microbiota can regulate local inflammatory responses and immune cell activity, thereby influencing both the tumor-killing effects and the extent of damage to normal tissues.
Advances in Research on the Relationship Between Gut Microbiota and Cancer
Identification of Key Microbial Species Influencing Cancer Therapy
In recent years, researchers have employed high-throughput sequencing and metagenomic analysis to explore the composition and functions of the gut microbiota in depth. This has led to the identification of several microbial species associated with cancer treatment response.
In addition to previously mentioned species like Bifidobacterium spp. and Fusobacterium nucleatum, Bacteroides fragilis has also been identified as a significant player. Studies from 2015 demonstrated that under therapeutic pressure, these bacterial species modulate antitumor immune responses. For instance, Bacteroides fragilis can secrete polysaccharide A, which helps balance immune function and enhance antitumor immunity.
Moreover, research indicates that specific combinations of bacterial strains may exert a greater influence on therapeutic outcomes than individual strains alone. This finding provides a theoretical basis for developing personalized microbiota-based cancer treatments.
Exploring Mechanisms of Gut Microbiota’s Influence on Cancer Therapy
As research progresses, the mechanisms by which gut microbiota influence cancer therapy outcomes are becoming clearer.
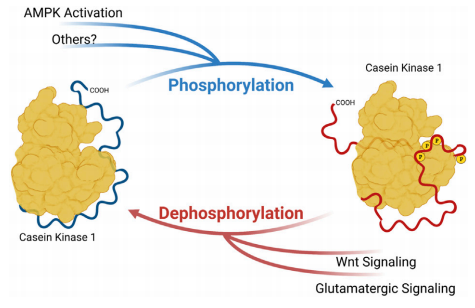
Besides immune modulation, gut microbiota can affect cancer development and treatment through various other pathways. For instance, gut microbes produce bioactive compounds such as short-chain fatty acids (SCFAs), bile acids, and vitamins. These metabolites can directly or indirectly affect tumor cell growth, proliferation, and apoptosis. SCFAs, for example, can regulate energy metabolism and gene expression in cells, suppressing tumor growth. Bile acids may activate signaling pathways that influence tumor proliferation and metastasis.
Additionally, gut microbiota may interact with receptors on the surface of tumor cells, thereby affecting their biological behavior. They may also alter the physicochemical properties of the tumor microenvironment—such as pH and redox balance—impacting tumor cell survival and progression.
Preliminary Clinical Findings
Although clinical research on the relationship between gut microbiota and cancer therapy is still in its early stages, some promising results have been reported.
Small-scale clinical trials have shown that regulating the gut microbiota—through probiotics, prebiotics, or fecal microbiota transplantation (FMT)—can improve cancer treatment outcomes and patient quality of life. For example, a study involving advanced lung cancer patients found that those who took oral probiotics alongside immune checkpoint inhibitors (ICIs) had a longer median progression-free survival compared to those receiving ICIs alone.
Another clinical study combining FMT with PD-1 inhibitors in patients with refractory solid tumors showed durable changes in gut microbiota and clinical benefits, with a notable objective response rate.
However, these studies were limited by small sample sizes and need to be validated by larger, well-controlled clinical trials.
Challenges and Future Research Directions
Challenges
Despite significant progress in research on the relationship between gut microbiota and cancer, several challenges remain.
First, the composition and function of gut microbiota are influenced by various factors such as diet, lifestyle, genetic background, and geographical differences. These variables make it difficult to reproduce and compare findings across different studies.
Second, the specific mechanisms by which gut microbiota influences cancer therapy responses are still not fully understood, and conflicting results exist among current studies, necessitating further in-depth research.
Moreover, translating basic research into clinical applications poses considerable challenges. Developing safe and effective microbiota-based cancer therapies requires resolving issues related to safety, efficacy, treatment timing, and protocol optimization. This is especially critical when applying probiotics, prebiotics, or fecal microbiota transplantation (FMT).
Future Research Directions
Future studies on the relationship between gut microbiota and cancer will likely focus on the following areas:
First, further elucidation of the molecular mechanisms through which gut microbiota modulates cancer therapy responses. This includes identifying key signaling pathways and molecular targets to support the development of novel treatments.
Second, conducting large-scale, multicenter clinical trials to evaluate the efficacy and safety of microbiota interventions in cancer therapy. This would also support personalized treatment strategies tailored to a patient’s specific microbiota profile and cancer type.
Third, the development of novel microbiota-modulating technologies and products. These may include engineered probiotic consortia or drugs based on microbial metabolites, aimed at enhancing specificity and effectiveness.
Fourth, a more integrative approach that considers interactions between gut microbiota and other factors—such as diet, lifestyle, and other treatment modalities—to formulate comprehensive and effective cancer prevention and therapy strategies.
Conclusion
In conclusion, there is a close and complex relationship between gut microbiota and cancer.
Gut microbiota can influence the onset, progression, and treatment efficacy of cancer through various mechanisms, particularly by regulating the immune system. In recent years, significant advances have been made in identifying key microbial species, exploring their mechanisms of action, and translating findings into clinical applications.
Despite these achievements, numerous challenges remain. The complexity of microbiota composition, individual variability, and limited clinical validation hinder immediate application.
Looking ahead, continued research and technological advancements are expected to lead to the development of novel, microbiota-based cancer therapies that offer new hope for patients. However, extensive basic and clinical research is still needed to ensure their safety and efficacy before clinical integration.
References
Iida, N., et al. (2013). Commensal bacteria control cancer response to therapy by modulating the tumor microenvironment. Science, 342, 967–970.
https://www.science.org/doi/abs/10.1126/science.1240527
Gopalakrishnan, V., et al. (2018). Gut microbiome modulates response to anti-PD-1 immunotherapy in melanoma patients. Science, 359, 97–103.