Semaglutide: Improving Lives through Glucose Control and Weight Reduction
Abstract
Semaglutide is a medication belonging to the class of glucagon-like peptide-1 receptor agonists (GLP-1 RAs). It is used for the management of type 2 diabetes mellitus and chronic weight management. By mimicking the effects of the hormone GLP-1, Semaglutide helps regulate blood sugar levels, stimulates insulin secretion, reduces glucagon release, and slows gastric emptying. These actions contribute to improved glycemic control and potential weight loss. Semaglutide is typically administered once weekly as a subcutaneous injection. It has shown efficacy in lowering HbA1c levels, aiding weight management, and reducing the risk of cardiovascular events.
What is Semaglutide
Semaglutide is a glucagon-like peptide-1 receptor agonist (GLP-1 RA) used in the treatment of type 2 diabetes and chronic weight management. By mimicking the actions of the hormone GLP-1, Semaglutide stimulates insulin release, lowers blood glucose levels, and promotes weight loss. It is administered once weekly via subcutaneous injections. In clinical trials, Semaglutide has shown effectiveness in reducing HbA1c levels, aiding weight management, and improving cardiovascular outcomes in people with diabetes. For chronic weight management, Semaglutide, in combination with lifestyle modifications, has led to significant weight loss. Common side effects include gastrointestinal symptoms. Overall, Semaglutide offers a promising therapeutic option for type 2 diabetes and weight management.
Mechanism of Action
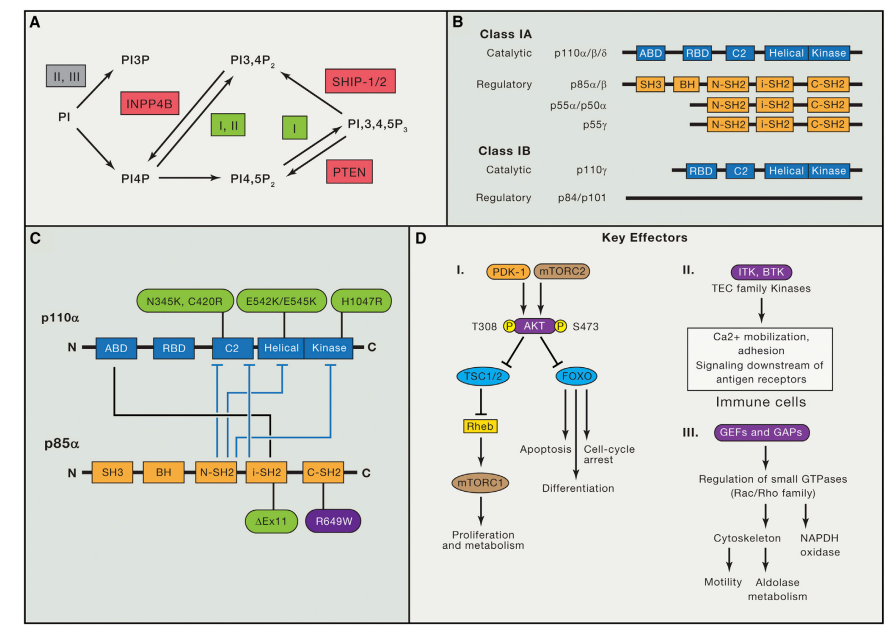
The mechanism of action of Semaglutide involves its interaction with glucagon-like peptide-1 (GLP-1) receptors in the body. Semaglutide is a synthetic analog of human GLP-1 and acts as a GLP-1 receptor agonist (GLP-1 RA).
When Semaglutide is administered, it binds to GLP-1 receptors located on various target tissues, including pancreatic beta cells, which are responsible for producing insulin. By binding to these receptors, Semaglutide activates intracellular signaling pathways that stimulate insulin secretion in response to elevated blood glucose levels. This increase in insulin helps lower blood sugar levels by facilitating the uptake of glucose by cells.
Fig. 1 Mechanism of semaglutide for management of obesity, NASH, and neurodegenerative diseases.
Semaglutide also has other effects beyond insulin secretion. It slows down gastric emptying, meaning food stays in the stomach for longer periods. This delayed gastric emptying can contribute to a feeling of fullness, reducing appetite and food intake.
Furthermore, Semaglutide decreases the production of glucose by the liver. By suppressing hepatic glucose output, Semaglutide helps lower fasting blood glucose levels and contributes to better glycemic control.
The combination of increased insulin secretion, delayed gastric emptying, and reduced hepatic glucose production collectively leads to improved glycemic control and can contribute to weight loss in individuals with type 2 diabetes or obesity.
It’s important to note that while Semaglutide acts primarily on GLP-1 receptors, it may also have additional effects on other receptors in the body, although their exact contributions to the medication’s overall mechanism of action are still being studied.
Overall, Semaglutide’s mechanism of action involves activating GLP-1 receptors, which leads to increased insulin secretion, delayed gastric emptying, reduced hepatic glucose production, and ultimately improved glycemic control and weight management.
Indications for Semaglutide
Semaglutide has two primary indications. Firstly, it is used for the treatment of type 2 diabetes mellitus to improve glycemic control. Secondly, Semaglutide is approved for chronic weight management in adults with a body mass index (BMI) of 30 or higher, or a BMI of 27 or higher with at least one weight-related comorbidity. In type 2 diabetes, Semaglutide helps lower blood glucose levels and reduces the risk of cardiovascular events. For chronic weight management, Semaglutide, in combination with lifestyle modifications, assists in achieving weight loss.
Use in Type 2 Diabetes Management
Semaglutide is widely used in the management of type 2 diabetes mellitus. It is administered as a once-weekly subcutaneous injection and acts as a glucagon-like peptide-1 receptor agonist (GLP-1 RA). By mimicking the effects of GLP-1, Semaglutide helps regulate blood sugar levels in multiple ways. It stimulates insulin secretion from pancreatic beta cells, reduces glucagon secretion, slows gastric emptying, and suppresses hepatic glucose production. These actions collectively result in improved glycemic control, lower HbA1c levels, and reduced fasting and postprandial blood glucose levels. Clinical studies have demonstrated the efficacy of Semaglutide in reducing the risk of cardiovascular events and promoting weight loss in people with type 2 diabetes. It is important to note that Semaglutide is typically used as part of a comprehensive diabetes management plan, which may include dietary modifications, exercise, and other antidiabetic medications.
Use in Chronic Weight Management
Semaglutide has been approved for use in chronic weight management in adults with obesity or overweight who have a body mass index (BMI) of 30 or higher, or a BMI of 27 or higher with at least one weight-related comorbidity. It is administered as a once-weekly subcutaneous injection. Semaglutide aids in weight management by acting as a glucagon-like peptide-1 receptor agonist (GLP-1 RA). It reduces appetite and increases the feeling of fullness by slowing gastric emptying and regulating the hunger centers in the brain. Clinical trials have shown that Semaglutide, when used in combination with lifestyle modifications, can lead to significant weight loss. It is important to note that Semaglutide should be used as part of a comprehensive weight management plan, which includes a healthy diet, increased physical activity, and behavior modifications.
Potential Side Effects
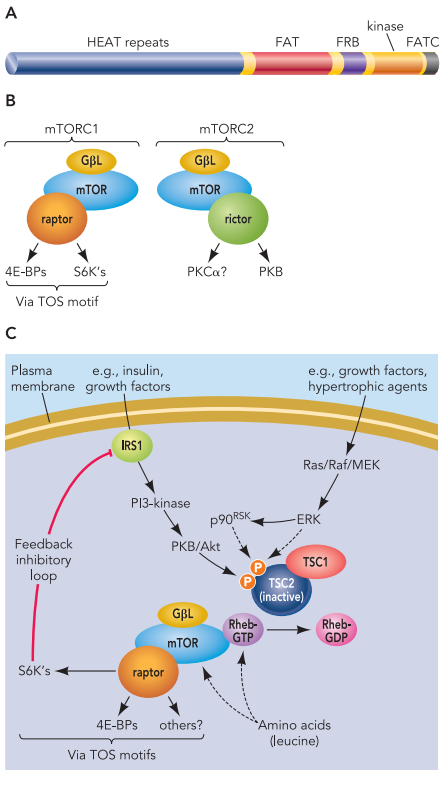
While Semaglutide is generally well-tolerated, there are potential side effects to be aware of. The most common side effects include gastrointestinal symptoms such as nausea, vomiting, and diarrhea. These symptoms are usually mild and tend to decrease over time. Less frequently reported side effects include abdominal pain, constipation, and decreased appetite. In rare cases, serious side effects such as pancreatitis and kidney problems may occur. It is important to promptly report any concerning symptoms to a healthcare professional.
Fig.2 Potential adverse effects associated with GLP1-RAs.
Clinical Efficacy and Research Findings
Clinical efficacy and research findings have demonstrated the effectiveness of Semaglutide in both type 2 diabetes management and chronic weight management.
In type 2 diabetes, numerous clinical trials have shown that Semaglutide significantly reduces HbA1c levels, a measure of long-term blood sugar control, when compared to placebo or other antidiabetic medications. It also helps lower fasting and postprandial blood glucose levels, leading to improved glycemic control. Additionally, Semaglutide has shown cardiovascular benefits by reducing the risk of major adverse cardiovascular events in people with diabetes.
In the context of chronic weight management, clinical studies have indicated that Semaglutide, when combined with lifestyle modifications, leads to significant weight loss compared to placebo. Research findings have shown that individuals treated with Semaglutide achieve greater reductions in body weight, BMI, and waist circumference. Furthermore, Semaglutide has demonstrated improvements in cardiometabolic risk factors, such as blood pressure and lipid profiles.
Overall, the clinical efficacy of Semaglutide suggests its effectiveness in addressing both diabetes and weight management. The medication’s ability to simultaneously improve glycemic control, aid weight loss, and provide cardiovascular benefits makes it a valuable therapeutic option.
Comparison with Other GLP-1 Receptor Agonists
When comparing Semaglutide with other GLP-1 receptor agonists (GLP-1 RAs), several factors come into play. One notable aspect is the dosing frequency. Semaglutide stands out as it is administered once weekly, offering convenience and potentially improving treatment adherence compared to other GLP-1 RAs that require daily or twice-daily dosing.
Another consideration is efficacy. Clinical studies have shown that Semaglutide achieves significant reductions in HbA1c levels and aids in weight loss comparable to or even superior to other GLP-1 RAs. For example, in head-to-head trials, Semaglutide has demonstrated greater weight loss outcomes when compared to other GLP-1 RAs.
Safety profiles are also important when evaluating GLP-1 RAs. While side effects such as gastrointestinal symptoms are common among GLP-1 RAs, including Semaglutide, the severity and frequency may vary among individuals. Overall, the safety profiles of different GLP-1 RAs are comparable, but specific side effects may differ slightly.
Cost and insurance coverage can also influence the choice of GLP-1 RA. Pricing and reimbursement policies may vary, and individual insurance plans may have specific formulary preferences.
Ultimately, the selection of a GLP-1 RA should be made in consultation with a healthcare professional, taking into account factors such as dosing convenience, efficacy, safety, individual patient characteristics, and insurance coverage to determine the most suitable option for an individual’s specific needs and goals.
Ongoing Research and Future Developments
Ongoing research and future developments in the field of Semaglutide continue to explore new avenues for its application and potential improvements. Here are a few areas of ongoing research and potential future developments:
Expanded Indications: Researchers are investigating the use of Semaglutide in additional patient populations, such as adolescents with type 2 diabetes or individuals with prediabetes, to assess its efficacy and safety in these groups.
Combination Therapies: Studies are being conducted to evaluate the efficacy and safety of combining Semaglutide with other antidiabetic medications or weight management drugs, aiming to achieve enhanced glycemic control and weight loss outcomes.
Long-Acting Formulations: Researchers are exploring the development of extended-release or longer-acting formulations of Semaglutide to reduce dosing frequency, potentially enhancing convenience and treatment adherence.
Cardiovascular Outcomes: Ongoing research aims to further understand the long-term cardiovascular benefits of Semaglutide and its impact on reducing the risk of major adverse cardiovascular events.
Personalized Medicine: Efforts are being made to identify biomarkers or genetic factors that may predict an individual’s response to Semaglutide, enabling personalized treatment approaches and optimizing outcomes.
Continued research and development in these areas hold the potential to further enhance the clinical efficacy, safety, and applicability of Semaglutide, providing more tailored and effective treatment options for individuals with type 2 diabetes and obesity.
References
- Anderson SL, Beutel TR, Trujillo JM. Oral semaglutide in type 2 diabetes. J Diabetes Complications. 2020 Apr;34(4):107520. doi: 10.1016/j.jdiacomp.2019.107520. Epub 2020 Jan 8. PMID: 31952996.
- Bucheit JD, Pamulapati LG, Carter N, Malloy K, Dixon DL, Sisson EM. Oral Semaglutide: A Review of the First Oral Glucagon-Like Peptide 1 Receptor Agonist. Diabetes Technol Ther. 2020 Jan;22(1):10-18. doi: 10.1089/dia.2019.0185. Epub 2019 Oct 1. PMID: 31436480.
- Andersen A, Knop FK, Vilsbøll T. A Pharmacological and Clinical Overview of Oral Semaglutide for the Treatment of Type 2 Diabetes. Drugs. 2021 Jun;81(9):1003-1030. doi: 10.1007/s40265-021-01499-w. Epub 2021 May 8. PMID: 33964002; PMCID: PMC8217049.
- Mahapatra MK, Karuppasamy M, Sahoo BM. Therapeutic Potential of Semaglutide, a Newer GLP-1 Receptor Agonist, in Abating Obesity, Non-Alcoholic Steatohepatitis and Neurodegenerative diseases: A Narrative Review. Pharm Res. 2022 Jun;39(6):1233-1248. doi: 10.1007/s11095-022-03302-1. Epub 2022 Jun 1. PMID: 35650449; PMCID: PMC9159769.
- Bergmann NC, Davies MJ, Lingvay I, Knop FK. Semaglutide for the treatment of overweight and obesity: A review. Diabetes Obes Metab. 2023 Jan;25(1):18-35. doi: 10.1111/dom.14863. Epub 2022 Oct 18. PMID: 36254579; PMCID: PMC10092086.
- Smits MM, Van Raalte DH. Safety of Semaglutide. Front Endocrinol (Lausanne). 2021 Jul 7;12:645563. doi: 10.3389/fendo.2021.645563. Erratum in: Front Endocrinol (Lausanne). 2021 Nov 10;12:786732. PMID: 34305810; PMCID: PMC8294388.