Pulmonary Nodules: Complete Guide to Diagnosis, Risk & Management
Abstract
Pulmonary nodules are small, round growths found in the lungs, often discovered incidentally during chest imaging. While most are benign, some can indicate early-stage lung cancer. This article provides an overview of pulmonary nodules, including their causes, diagnostic techniques such as CT and PET scans, risk factors for malignancy, and management strategies. It also outlines when follow-up is necessary and how to interpret key imaging findings. With proper evaluation and monitoring, most pulmonary nodules can be managed safely, reducing patient anxiety and avoiding unnecessary procedures.
What Are Pulmonary Nodules?
Pulmonary nodules are small, rounded growths or spots that appear in the lungs, typically discovered incidentally during imaging tests such as a chest X-ray or a computed tomography (CT) scan. These nodules are usually less than 3 centimeters (about 1.2 inches) in diameter. When larger than this, they are referred to as pulmonary masses, which may carry a higher risk of malignancy.
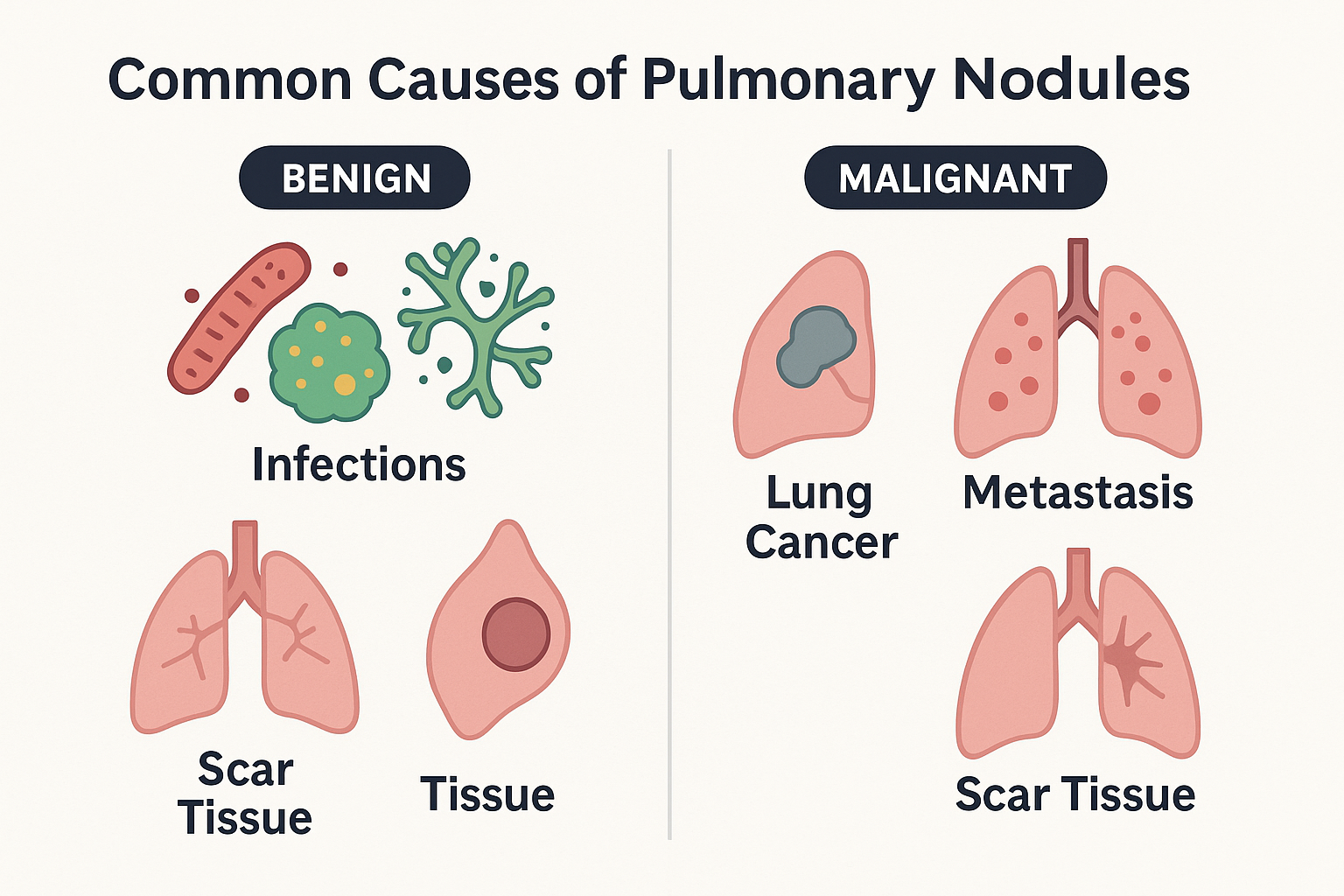
Most pulmonary nodules are benign, meaning they are non-cancerous. These may result from previous infections (such as tuberculosis or fungal infections), scar tissue, or inflammation. However, some nodules can be malignant, representing early stages of lung cancer or metastasis from cancers elsewhere in the body. Distinguishing between benign and malignant nodules is crucial and often requires further imaging or biopsy.
There are different types of pulmonary nodules based on how they appear on imaging. Solid nodules are completely opaque on scans, while subsolid nodules—including ground-glass nodules (GGNs)—are partially transparent and may indicate more complex underlying processes, such as atypical adenomatous hyperplasia or early-stage lung adenocarcinoma.
Pulmonary nodules are generally asymptomatic and do not cause noticeable health issues on their own. Most are discovered when imaging is performed for another reason. Still, their presence often leads to anxiety and the need for careful follow-up, especially in individuals with risk factors such as smoking, advanced age, or a history of cancer.
Understanding what pulmonary nodules are—and what they are not—is a critical first step toward appropriate evaluation and management.
Common Causes of Pulmonary Nodules
Pulmonary nodules can develop for a variety of reasons, some of which are non-cancerous, while others may suggest malignancy. Understanding the causes is crucial for determining whether a nodule poses a health risk.
 Benign Causes
Benign Causes
The majority of pulmonary nodules are benign and typically result from previous infections or inflammatory processes. One of the most common causes is granulomas, which are small areas of inflammation formed when the body’s immune system responds to infections like tuberculosis (TB) or fungal infections. In fact, granulomas are often the result of past infections that have resolved without causing ongoing symptoms.
Another benign cause is scar tissue from prior lung injuries or diseases. For example, if a person had pneumonia or another lung infection in the past, scar tissue may form, leading to a nodule-like appearance on scans. Hamartomas, which are benign tumors made of normal tissue in abnormal amounts, can also form nodules, though they rarely cause health problems.
Malignant Causes
In some cases, pulmonary nodules may signal more serious conditions. Lung cancer is the most significant concern, particularly if the nodule grows or changes over time. Primary non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC) can both present as solitary pulmonary nodules.
Metastasis from cancers that originated in other parts of the body, such as the breast, colon, or kidney, is another major cause of malignant nodules. These metastatic tumors often show up as multiple nodules in the lungs and require aggressive treatment and close monitoring.
While most pulmonary nodules are benign, their size, shape, and growth rate over time provide crucial clues to their potential malignancy, making timely follow-up essential for accurate diagnosis.
How Pulmonary Nodules Are Diagnosed
Diagnosing pulmonary nodules accurately is essential for determining whether they are benign or malignant. Since nodules are typically discovered incidentally—during imaging for unrelated health issues—the diagnostic process is focused on assessing risk, monitoring changes, and deciding if further testing is needed.
 Imaging Techniques
Imaging Techniques
The most common initial diagnostic tool is the chest CT scan, which provides detailed images of the lungs and allows for measurement of the nodule’s size, shape, density, and growth. A key advantage of CT is its ability to detect subtle features, such as spiculated margins, calcification, or ground-glass opacities, all of which may offer clues about malignancy.
For more suspicious nodules, a PET scan (positron emission tomography) may be recommended. PET scans can detect metabolic activity—cancerous nodules often consume more glucose and appear “hot” on these scans.
Biopsy and Tissue Sampling
If imaging suggests malignancy or if a nodule is growing, a biopsy may be performed. This can be done via CT-guided needle biopsy, bronchoscopy, or surgical biopsy. The collected tissue is analyzed under a microscope to confirm the presence of cancer cells.
Emerging Diagnostic Tools
Recent advances in diagnostic technology include blood-based biomarkers (e.g., circulating tumor DNA, miRNA panels), and radiomics, which uses AI to analyze imaging data. These tools are especially useful when biopsy is risky or not feasible.
Combining imaging findings with clinical risk models—such as the Brock model or the Mayo Clinic model—helps determine the likelihood of malignancy and guide appropriate follow-up.
Are Pulmonary Nodules Dangerous? Understanding the Risks
The discovery of a pulmonary nodule can be alarming, especially when cancer is a concern. However, not all pulmonary nodules are dangerous. Many are benign, particularly in individuals without major risk factors. The key is identifying which nodules require further investigation and which can be safely monitored.
Risk Factors That Increase Concern
Certain characteristics make a pulmonary nodule more likely to be malignant:
Size: Nodules larger than 8 mm carry a higher risk of cancer.
Growth: Nodules that increase in size over time are more suspicious.
Borders: Irregular or spiculated edges are more concerning than smooth margins.
Location: Upper lobe nodules are more commonly associated with malignancy.
Patient History: Smoking, older age, a personal or family history of cancer, or exposure to harmful substances (like asbestos or radon) significantly increase risk.
Nodules that remain stable for over 2 years on imaging are generally considered benign, especially if they are small and lack aggressive features.
Malignancy Rates and Probability Models
Statistical models—such as the Mayo Clinic model or the Brock University model—help predict the likelihood that a pulmonary nodule is malignant based on clinical and imaging data. According to studies, about 60–80% of nodules detected in smokers over 50 are benign, but a cautious approach is still necessary.
Surveillance vs. Biopsy
Low-risk nodules are usually followed with serial CT scans to monitor stability. High-risk nodules may warrant a biopsy or PET scan to rule out malignancy early.
Understanding the risk factors and diagnostic features is essential in determining the next steps—and whether aggressive intervention is necessary.
What to Do If You Have a Pulmonary Nodule
If you or your doctor discovers a pulmonary nodule, the next steps involve understanding its potential risk, determining the best course of action, and ensuring ongoing monitoring. While most nodules are benign, it’s important to carefully evaluate their characteristics to determine whether they require immediate intervention or can simply be monitored.
Follow-Up Imaging
The first step is typically surveillance imaging to track any changes in the nodule’s size or appearance. The frequency and type of imaging depend on the nodule’s size, location, and risk factors. For benign nodules, a follow-up CT scan every 6 to 12 months for 2 years is common. If the nodule remains stable over time, the likelihood of malignancy is low, and no further action may be required.
Biopsy or Further Testing
If there is concern that the nodule might be cancerous, your doctor may recommend a biopsy or PET scan. A CT-guided biopsy allows a tissue sample to be extracted for analysis, while a PET scan can assess the metabolic activity of the nodule to identify cancerous growth.
Lifestyle Modifications and Risk Reduction
For individuals with known risk factors—such as smoking or a family history of cancer—discussing lifestyle modifications is crucial. Smoking cessation is the most effective way to reduce the risk of developing further nodules or lung cancer. In addition, enrolling in a lung cancer screening program with low-dose CT is advised for high-risk individuals.
Stay Calm and Discuss Options
It’s important to stay calm. Most nodules are not cancerous, and many will remain stable or even shrink over time. Regular consultations with your doctor, proper monitoring, and understanding the situation can help alleviate anxiety.
References
MacMahon, H., Naidich, D. P., Goo, J. M., Lee, K. S., Leung, A. N., Mayo, J. R., … & Yankelevitz, D. F. (2017). Guidelines for management of incidental pulmonary nodules detected on CT images: from the Fleischner Society 2017. Radiology, 284(1), 228-243.
https://pubs.rsna.org/doi/full/10.1148/radiol.2017161659
Mazzone, P. J., & Lam, L. (2022). Evaluating the patient with a pulmonary nodule: a review. JAMA, 327(3), 264-273.
https://jamanetwork.com/journals/jama/article-abstract/2788136
Gould, M. K., Donington, J., Lynch, W. R., Mazzone, P. J., Midthun, D. E., Naidich, D. P., & Wiener, R. S. (2013). Evaluation of individuals with pulmonary nodules: when is it lung cancer? Diagnosis and management of lung cancer. Chest, 143(5), e93S-e120S.
https://www.sciencedirect.com/science/article/abs/pii/S0012369213602913
Wen, M., Zheng, Q., Ji, X., Xin, S., & Zhou, Y. (2024). Precise diagnosis and prognosis assessment of malignant lung nodules: A narrative review. Journal of Thoracic Disease.
https://pmc.ncbi.nlm.nih.gov/articles/PMC11635230/
Xu, S., Ge, J., Liu, X., He, Q., Xu, D., & Cao, W. (2023). The predictive value of chest computed tomography images, tumor markers, and metabolomics in the identification of benign and malignant pulmonary nodules. Journal of Thoracic Disease, 15(5), 2668-2679.
https://pmc.ncbi.nlm.nih.gov/articles/PMC10267948/
Cronin, P., et al. (2008). Solitary pulmonary nodules: meta-analytic comparison of cross-sectional imaging modalities. Radiology, 246(3), 772–782.
https://pubs.rsna.org/doi/abs/10.1148/radiol.2463062148
Mazzone, P. J., et al. (2021). Integrated biomarkers for the management of indeterminate pulmonary nodules. American Journal of Respiratory and Critical Care Medicine, 204(10), 1183–1192.
https://www.atsjournals.org/doi/full/10.1164/rccm.202012-4438OC




