Perphenazine: Uses, Side Effects, and What You Need to Know
Abstract
Perphenazine is a typical antipsychotic medication used primarily to treat schizophrenia and severe nausea or vomiting. It functions by blocking dopamine receptors in the brain, helping reduce psychotic symptoms. While effective, it may cause side effects such as extrapyramidal symptoms, sedation, and cardiovascular risks. Proper dosage, careful monitoring, and medical supervision are crucial for safe and effective use. This blog provides an overview of Perphenazine’s mechanism, clinical applications, safety concerns, and administration guidelines for both patients and healthcare providers.
Introduction to Perphenazine
Perphenazine is a typical antipsychotic medication that has been in clinical use since the 1950s. Belonging to the phenothiazine class, it is primarily prescribed for managing symptoms of schizophrenia, a chronic mental disorder characterized by hallucinations, delusions, and disorganized thinking. Although newer atypical antipsychotics have become more popular in recent years, Perphenazine remains a valuable option for certain patients due to its cost-effectiveness and efficacy in treating positive psychotic symptoms.
This medication works by altering the levels of dopamine in the brain—specifically by blocking D2 dopamine receptors. By doing so, it helps reduce the intensity of psychotic symptoms and can stabilize mood and thought processes. Aside from its use in psychiatric conditions, Perphenazine is also approved for controlling severe nausea and vomiting, especially in post-operative or chemotherapy contexts.
Patients who are prescribed Perphenazine often require close monitoring due to potential side effects, including movement disorders known as extrapyramidal symptoms (EPS), sedation, or anticholinergic effects like dry mouth and blurred vision. However, with careful dose adjustment and clinical oversight, many individuals benefit greatly from this medication.
As with all psychotropic medications, Perphenazine should only be used under the supervision of a qualified healthcare provider. Understanding the drug’s profile, benefits, and risks is essential not only for patients but also for caregivers and medical professionals.
How Perphenazine Works
Perphenazine functions by modulating neurotransmitter activity in the brain—specifically targeting dopamine, a chemical messenger critical to thought, emotion, and behavior. The drug acts as a dopamine D2 receptor antagonist, meaning it binds to and blocks these receptors, primarily in areas of the brain associated with psychotic symptoms, such as the mesolimbic and mesocortical pathways.
In people with schizophrenia and related disorders, overactivity of dopamine transmission in certain brain regions is believed to contribute to hallucinations, paranoia, and disordered thinking. By blocking dopamine’s effects, Perphenazine reduces the intensity of these symptoms and helps restore a more balanced mental state.
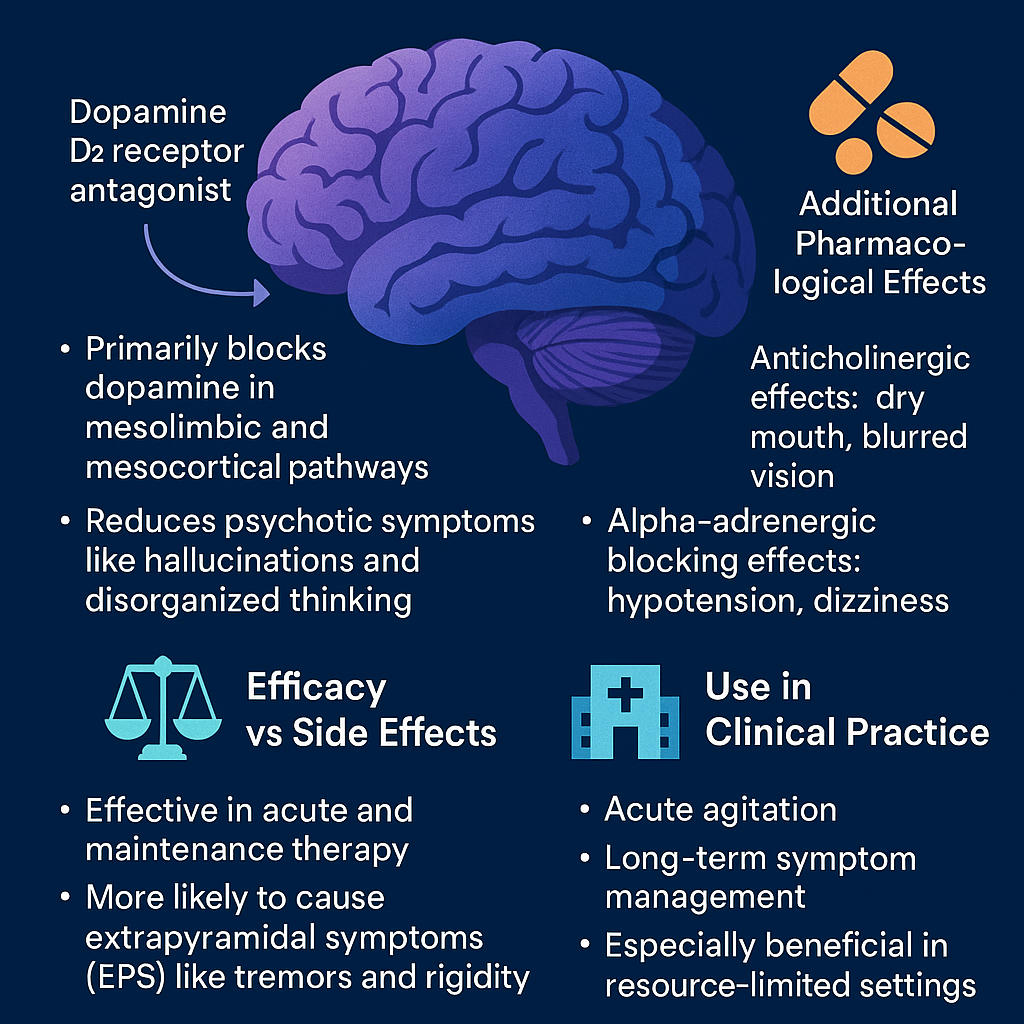
In addition to its dopamine-blocking properties, Perphenazine has anticholinergic, antihistaminic, and alpha-adrenergic blocking effects. These contribute to both therapeutic outcomes and side effects. For instance, the antihistaminic activity can cause sedation, while the anticholinergic action may lead to dry mouth and blurred vision.
Compared to newer atypical antipsychotics, Perphenazine is more likely to cause extrapyramidal symptoms (EPS), such as muscle stiffness or tremors. However, it tends to have a lower risk of weight gain, diabetes, and lipid abnormalities, which are common issues with many second-generation drugs.
Perphenazine’s multi-receptor profile makes it effective for acute agitation and ongoing symptom management, especially in resource-limited settings. Its onset of action is typically within hours, and its duration lasts 8–12 hours, making it suitable for both acute and maintenance therapy when properly managed.
Approved Medical Uses of Perphenazine
Perphenazine is primarily approved for the treatment of schizophrenia, a complex psychiatric disorder marked by symptoms like hallucinations, delusions, disorganized speech, and impaired cognitive function. It is especially effective in managing the positive symptoms of schizophrenia—those that involve an excess or distortion of normal functions, such as auditory hallucinations or paranoia.
Perphenazine is also used for controlling severe nausea and vomiting, especially when other antiemetics have failed. Its ability to block dopamine in the chemoreceptor trigger zone (CTZ) of the brain makes it effective for preventing emesis (vomiting), particularly in post-operative patients and those undergoing chemotherapy.
While not approved for these conditions, Perphenazine has also been used off-label in cases of acute agitation, bipolar disorder, and severe anxiety, often in combination with other medications. However, such use requires careful clinical judgment due to its potential for side effects.
Because of its potent antipsychotic effects and relatively lower cost, Perphenazine remains a common choice in many healthcare systems, especially in public mental health facilities and resource-limited environments. It may be prescribed as part of a long-term maintenance strategy or during the acute phase of psychosis.
Patients undergoing treatment with Perphenazine are typically monitored for therapeutic response and adverse effects, with dosage adjusted accordingly. It’s also frequently included in formulary options for hospitals and psychiatric care units, especially when managing chronic schizophrenia.
Side Effects and Warnings of Perphenazine
Like all antipsychotic medications, Perphenazine carries the potential for both common and serious side effects. Understanding these risks is essential for patients and caregivers to ensure safe use and timely intervention when necessary.
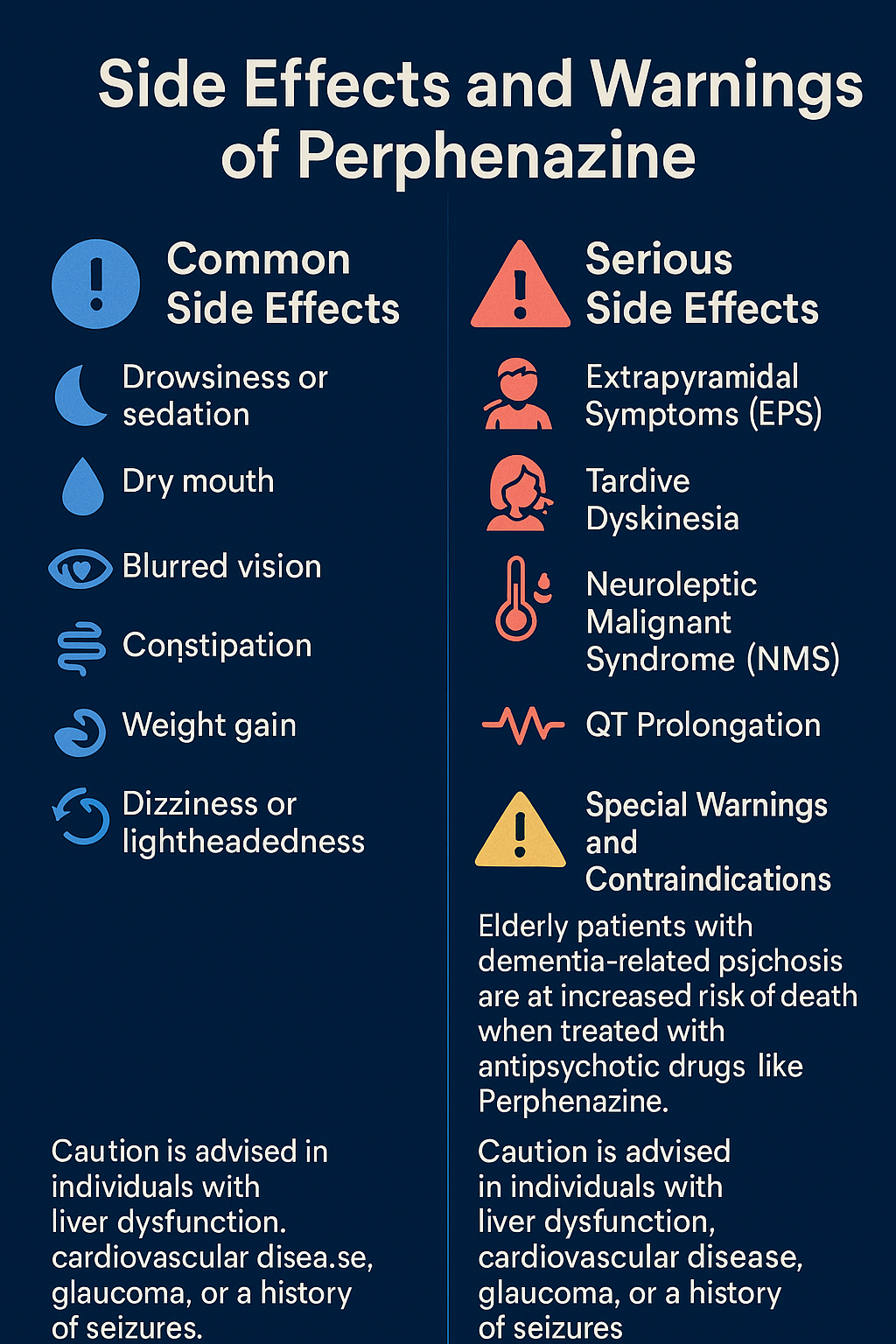
Common Side Effects
Most patients will experience some mild to moderate side effects, especially during the initial treatment phase. These include:
Drowsiness or sedation
Dry mouth
Blurred vision
Constipation
Weight gain
Dizziness or lightheadedness
These are generally manageable but should be reported to a healthcare provider if persistent or bothersome.
Serious Side Effects
Some adverse reactions require immediate medical attention:
Extrapyramidal Symptoms (EPS): These are drug-induced movement disorders such as tremors, rigidity, dystonia (muscle spasms), and akathisia (restlessness).
Tardive Dyskinesia: A potentially irreversible condition involving involuntary facial and limb movements. Risk increases with long-term use.
Neuroleptic Malignant Syndrome (NMS): A rare but life-threatening emergency involving high fever, muscle stiffness, confusion, and unstable blood pressure.
QT Prolongation: Perphenazine may affect heart rhythm, increasing the risk of a potentially fatal arrhythmia.
Special Warnings and Contraindications
Elderly patients with dementia-related psychosis are at increased risk of death when treated with antipsychotic drugs like Perphenazine.
Caution is advised in individuals with liver dysfunction, cardiovascular disease, glaucoma, or a history of seizures.
Drug interactions can occur, especially with central nervous system depressants, anticholinergic agents, and other dopaminergic antagonists.
Dosage, Administration, and Precautions of Perphenazine
Perphenazine is available in multiple forms, including oral tablets and injectable solutions, allowing flexibility depending on the patient’s condition and clinical setting. It should always be prescribed and adjusted by a healthcare provider, as dosage varies based on diagnosis, age, severity of symptoms, and patient response.
Typical Dosage Guidelines
Schizophrenia (Adults): The usual starting dose ranges from 4 to 8 mg two to three times daily, with a typical maintenance dose of 12–24 mg/day. The maximum recommended oral dose is 64 mg/day, though most patients respond to lower amounts.
Nausea/Vomiting (Short-Term Use): Typically, 8–16 mg/day in divided doses is sufficient.
For injectable use, Perphenazine is administered intramuscularly (IM) for rapid symptom control in acute psychotic episodes or severe nausea, usually in doses of 5–10 mg every 6–8 hours as needed.
Administration Tips
Tablets may be taken with or without food.
Consistent dosing times improve therapeutic outcomes.
Avoid abrupt discontinuation to prevent withdrawal or symptom rebound.
Important Precautions
Elderly patients: Increased risk of cerebrovascular events and mortality.
Pregnancy: Should only be used if benefits outweigh risks. Avoid during third trimester due to neonatal withdrawal risks.
Hepatic impairment: Use cautiously as the drug is metabolized by the liver.
Drug Interactions: Avoid alcohol, opioids, and other CNS depressants; may amplify sedative effects.
Patients should undergo regular monitoring, including liver function tests, ECG for cardiac health, and assessments for extrapyramidal symptoms.
Conclusion
Perphenazine remains a valuable antipsychotic medication with decades of clinical use in treating schizophrenia and controlling severe nausea and vomiting. Though it carries risks like extrapyramidal symptoms and sedation, it offers effective symptom control, especially when newer antipsychotics may be unsuitable or unaffordable. Understanding its mechanism, proper use, side effects, and precautions empowers patients and caregivers to make informed decisions. As with any psychiatric medication, medical supervision is essential to balance benefits with safety. If you’re considering or currently prescribed Perphenazine, always consult your healthcare provider for personalized guidance and monitoring. With responsible use, Perphenazine can play a key role in achieving stability and improved quality of life for many individuals.
References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing.
https://books.google.co.kr/books?hl=en&lr=&id=80zYBAAAQBAJ&oi=fnd&pg=RA1-PA9&dq=American+Psychiatric+Association.+(2013).+Diagnostic+and+statistical+manual+of+mental+disorders+(5th+ed.).+Arlington,+VA:+American+Psychiatric+Publishing.&ots=P2246qUnoS&sig=qjthSLolXAZRXs0KRMTFQ1NODDA&redir_esc=y#v=onepage&q&f=false
Muench, J., & Hamer, A. M. (2010). Adverse effects of antipsychotic medications. American Family Physician, 81(5), 617–622.
https://www.aafp.org/pubs/afp/issues/2010/0301/p617.html/1000
Lieberman, J. A., Stroup, T. S., McEvoy, J. P., et al. (2005). Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. New England Journal of Medicine, 353(12), 1209–1223.
https://www.nejm.org/doi/full/10.1056/NEJMoa051688
Miyamoto, S., Duncan, G. E., Marx, C. E., & Lieberman, J. A. (2005). Treatments for schizophrenia: A critical review of pharmacology and mechanisms of action of antipsychotic drugs. Molecular Psychiatry, 10(1), 79–104.
https://www.nature.com/articles/4001556
Kapur, S., & Mamo, D. (2003). Half a century of antipsychotics and still a central role for dopamine D2 receptors. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 27(7), 1081–1090.
https://www.sciencedirect.com/science/article/abs/pii/S0278584603002173
Seeman, P. (2002). Atypical antipsychotics: Mechanism of action. Canadian Journal of Psychiatry, 47(1), 27–38.
https://journals.sagepub.com/doi/abs/10.1177/070674370204700105