How does Adenosine Work?
Abstract
Adenosine is composed of adenine and ribose with a molecular weight of 267. Adenosine can participate in coronary vasodilation, increased blood flow, myocardial energy metabolism, and other processes. It has certain physiological effects on the cardiovascular system and many other systems of the body. Its source is mainly the hydrolysis of adenosine triphosphate (ATP) and the enzymatic hydrolysis of nucleotides and S-adenosylhomocysteine. The metabolism of adenosine can be divided into two pathways: adenosine deaminase and phosphorylase are two key enzymes in this metabolic process. Most of the adenosine will be rapidly degraded into xanthines under the action of this enzyme, and then transformed into uric acid. Excretion, a small part of adenosine can enter the cell again, synthesize ATP under the action of adenosine kinase, and then re-hydrolyze into adenosine; only a small amount of adenosine can be excreted directly through the kidney. It is precise because adenosine has a rapid metabolic system, making adenosine in the body’s very short half-life, about 0.5-10 s. Adenosine’s primary purpose is to reduce tissue damage and participate in different receptor-mediated responses, including increasing oxygen supply/demand ratios, ischemic preconditioning, anti-inflammatory effects, and promoting angiogenesis and increased or decreased capillary density. In 1930, scientists Honey and Ritchie first proposed the exogenous adenosine on human electrophysiological effects, adenosine on human basic and clinical research began. Adenosine and its derivatives have been widely used in infection, autoimmune, ischemic and degenerative diseases.
Adenosine action receptors
As an endogenous nucleoside widely present in human tissues, adenosine participates in various physiological and biochemical processes throughout the body by activating specific membrane receptors of adenosine receptors. Adenosine receptors are generally present in the brain, heart, kidney, blood vessels, adipose tissue, and platelets. According to their molecular and biochemical properties, the receptors are divided into four subtypes: A1R, A2aR, A2bR, and A3R. AIR is distributed throughout the body but mainly in the central system, such as hippocampus, cerebral cortex, and cerebellum. A2a levels were higher in the striatum and spleen of the brain, followed by heart, lung, and blood vessels; although A2bR is widely expressed in various tissues, the expression level is low, mainly distributed in vascular endothelial cells. A3 receptors are distributed in the body but are mainly expressed in the lungs and arteries.
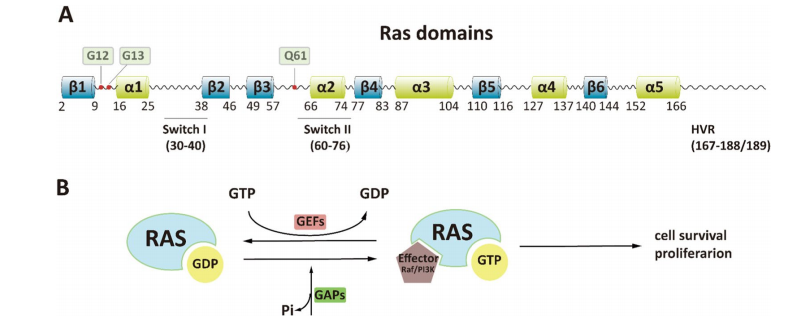
Adenosine receptors are coupled to G proteins and regulate the second messenger system by activating/inhibiting adenylate cyclase, which in turn triggers a series of signal-regulated cell functions. A2a/A2b binds to Gs protein. When endogenous ligand adenosine is present, adenylate cyclase is activated, making ATP dephosphorylation into cAMP: The increase in cAMP concentration activates Protein Kinase A (PKA), which activates calcium channels on the cell membrane, promotes extracellular calcium influx, and increases intracellular calcium concentration. A1/A3 binds to Gi protein, inhibits adenylate cyclase, and decreases cAMP concentration. On the other hand, A1 can also bind to Go protein to open potassium channels. A2B and A3 bind to Gq protein and activate phospholipase C (PLC) to produce messenger molecules: Diacylglycerol (DAG) and Inositol (1,4,5) -trisphosphate (IP3). Both increase protein kinase C (PKC) and intracellular calcium concentration, causing signal transduction.
At the cellular level, A1R and A3R are coupled to the Gi protein that inhibits cAMP production, while A2aR and A2bR are coupled to the Gs protein that activates adenylate cyclase, further promoting cAMP production. In the cardiovascular system, adenosine also protects myocardial/reperfusion injury by activating A1 and A3. A2aR and A2bR strongly act on coronary blood flow (CBF). The four receptors of adenosine belong to the G protein spiral transmembrane receptor family. The difference is that the signal transmitted by A1R and A3R is the inhibition of adenylate cyclase (AC). The affinity of A2aR is much higher than that of A2bR, and A2aR and A2bR activate adenylate cyclase by stimulating Gs protein.
The role of adenosine
Adenosine as an endogenous nucleoside throughout the body cells, at low concentrations, can inhibit the parasympathetic nerve to accelerate heart rate; high concentration of adenosine can inhibit sinoatrial node and atrioventricular conduction, resulting in atrioventricular block and bradycardia. In addition, adenosine also has anti-adrenergic effects and vasodilatory effects on all arteries except the anterior glomerular artery. Although the role of adenosine in the regulation of normal coronary arteries has not been conclusive, the important role of adenosine as a regulator of blood flow is particularly prominent during ischemia/oxygen. In addition, adenosine can increase cardiac output and coronary blood flow, increase pulmonary artery pressure, and reduce ventricular compliance.
Under the stimulation of ischemia, hypoxia, or inflammation, the concentration of adenosine in local cells or tissues will increase to regulate the ATP metabolism of local tissues, protect them from external factors, promote angiogenesis, and increase capillary density. In addition, adenosine also plays an important role in the regulation of skeletal muscle blood flow: adenosine production is significantly increased in the case of muscle contraction, ischemia, or systemic hypoxia. Adenosine production is also significantly increased during tissue ischemia and binds to receptors on the arterial smooth muscle cell membrane to cause vasodilation. Adenosine can not only induce vasodilation by directly acting on adenosine receptors on vascular cells but also cause the release of vasoactive substances potassium and vasodilator factors by acting on adenosine receptors on skeletal muscle cell membranes: The increased signal of ADP causes the opening of K+ channels to cause potassium to flow outward, thereby increasing membrane potential in smooth muscle cells. This hyperpolarization causes the voltage-dependent Ga channel to close; the resulting decrease in intracellular calcium produces relaxation of vascular smooth muscle and vasodilation. ATP-sensitive potassium channel (K+-ATP) and calcium-activated potassium channel (K+-Ca2+) are abundantly expressed in arterial smooth muscle, which helps to regulate blood flow. In addition, in terms of regulating blood flow and vascular function, adenosine and vasodilator nitric oxide (NO) also interact with each other. Adenosine binds to A2a and A2b receptors to enhance the role of vascular smooth muscle vasodilators, which in turn affects NO production.
At present, more research on adenosine is its vasodilation effect, but now its ‘steal effect’ has been gradually applied to clinical. It is well known that in the basic state, dilation of the resistance vessel zone compensates the collateral resistance vessels to maintain adequate blood flow. However, in the case of increased tissue oxygen demand (exercise) or the use of vasodilator (adenosine) load, increased arterial blood flow increases the pressure drop in the stenosis area, resulting in a decrease in pressure in the normal artery and collateral area. If the pressure drop of the blood supply artery exceeds the ability of the collateral resistance vessel to dilate, the blood flows into the collateral area will be reduced. As a common vasodilator, adenosine can cause rapid expansion of normal arteries, while the blood vessels in the narrow area cannot relax as normal blood vessels do, so the blood flows from the ischemic area to the non-ischemic area, resulting in ‘ arterial steal ‘ effect. The blood flow distribution in the ischemic area and the non-ischemic area is more obvious, which can be applied to the early diagnosis of vascular disease. Of course, adenosine can also bring some side effects. Adenosine can cause adverse reactions such as accelerated heart rate, palpitations, sweating, etc. However, due to its half-life of only 5-10s, the adverse reactions will disappear within seconds to 1-2min after withdrawal, so it is not necessary to give antagonists. Therefore, the use of adenosine as a diagnostic reagent has become a research hotspot for many scholars at home and abroad in recent years.
Adenosine is mainly used as a drug for the treatment of cardiovascular diseases in the market. It is worth noting that some anti-cancer clinical trials of adenosine have been carried out or are in progress, such as the phase II clinical trial of adenosine in the treatment of liver cancer. The anticancer mechanism of adenosine mainly involves endogenous and exogenous signaling pathways. In summary, adenosine has broad application prospects in anticancer therapy. In addition to adenosine, its analogues have also been shown to inhibit cancer progression. For example, acadipine, fludarabine phosphate, and clofarabine have been officially approved as anti-leukemia anticancer drugs. In addition, the anticancer activities of cladribine, 8-chloroadenosine (8-C1-Ado), and pentostatin have also been verified in clinical trials.