Eliquis (Apixaban): What It Is, How It Works, and Who Should Take It
Abstract
This blog post offers a comprehensive overview of Eliquis (apixaban), a widely prescribed oral anticoagulant used to prevent blood clots in patients with conditions such as non-valvular atrial fibrillation, deep vein thrombosis (DVT), and pulmonary embolism (PE). The article explores the drug’s mechanism of action, pharmacological benefits, ideal patient profiles, potential side effects, drug interactions, and its FDA-approved reversal agent. Readers will also find practical advice on safe usage, common patient questions, and how Eliquis compares to traditional anticoagulants like warfarin. Designed for both patients and healthcare consumers, the post aims to improve understanding and confidence in managing anticoagulation therapy.
Introduction to Eliquis (Apixaban)
Eliquis, the brand name for apixaban, is a widely prescribed oral anticoagulant used to reduce the risk of blood clots. It belongs to a class of medications known as direct oral anticoagulants (DOACs), specifically a Factor Xa inhibitor, which helps prevent clot formation by blocking one of the key proteins in the coagulation cascade.
Approved by the FDA in 2012, Eliquis is commonly prescribed for people with non-valvular atrial fibrillation (AFib)—a heart rhythm disorder that increases the risk of stroke. It is also used to treat and prevent deep vein thrombosis (DVT) and pulmonary embolism (PE), and to reduce clot risk after hip or knee replacement surgery.
What sets Eliquis apart is its predictable pharmacokinetics, fixed dosing, and lower risk of serious bleeding compared to older anticoagulants like warfarin. Unlike warfarin, Eliquis does not require routine INR blood monitoring or strict dietary restrictions, making it a more convenient choice for many patients.
Its rapid onset and offset make it particularly beneficial for managing clot risks without long delays. Patients appreciate its simplicity, and physicians value its evidence-based safety and efficacy in both clinical trials and real-world use.
As the use of DOACs continues to rise globally, Eliquis remains one of the most prescribed and trusted options in its class. Understanding how it works and why it’s chosen over other blood thinners is essential for informed decision-making and improved health outcomes.
How Eliquis Works: Mechanism and Science Explained
Eliquis (apixaban) is part of a newer class of blood thinners known as direct oral anticoagulants (DOACs). Unlike older medications like warfarin, which interfere with vitamin K-dependent clotting factors, Eliquis works by selectively inhibiting Factor Xa, an essential enzyme in the clotting cascade.
To understand this, consider how blood clots form: when there is injury to a blood vessel, a series of reactions occur to produce thrombin, which converts fibrinogen into fibrin, forming a blood clot. Factor Xa plays a critical role in this process by converting prothrombin to thrombin. By directly blocking Factor Xa, apixaban prevents thrombin generation, reducing clot formation without entirely shutting down the body’s ability to stop bleeding when needed.
Eliquis is absorbed quickly, reaching peak concentration within 3–4 hours of ingestion. Its half-life is about 12 hours, which supports twice-daily dosing and allows for steady anticoagulant effects with minimal fluctuations. It is metabolized primarily by the liver (CYP3A4 pathway) and partially eliminated through the kidneys, making it a suitable option even for patients with mild to moderate kidney impairment.
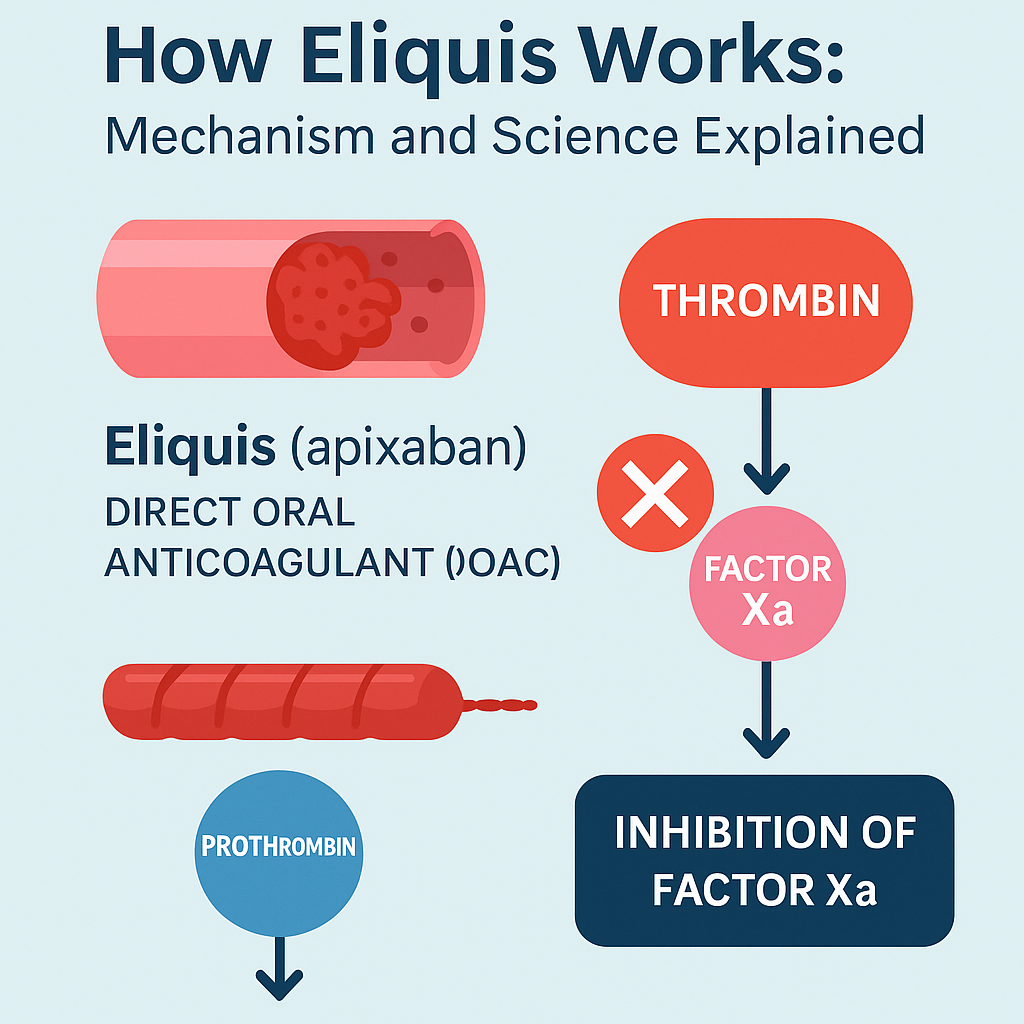
A key advantage of this mechanism is that it does not require routine blood monitoring, as the anticoagulation effect is predictable across most patients. Moreover, because Eliquis targets only one step in the clotting cascade, it tends to cause less major bleeding, especially in the brain, compared to older therapies like warfarin.
This focused mechanism makes Eliquis a preferred anticoagulant in many clinical scenarios, offering a balance between efficacy and safety.
Who Should Take Eliquis (and Who Shouldn’t?)
Eliquis (apixaban) is prescribed to reduce the risk of stroke, blood clots, and systemic embolism in certain high-risk individuals. Its targeted action and user-friendly dosing make it a first-line option in many situations, but it is not suitable for everyone.
Who Should Take Eliquis?
Eliquis is typically recommended for:
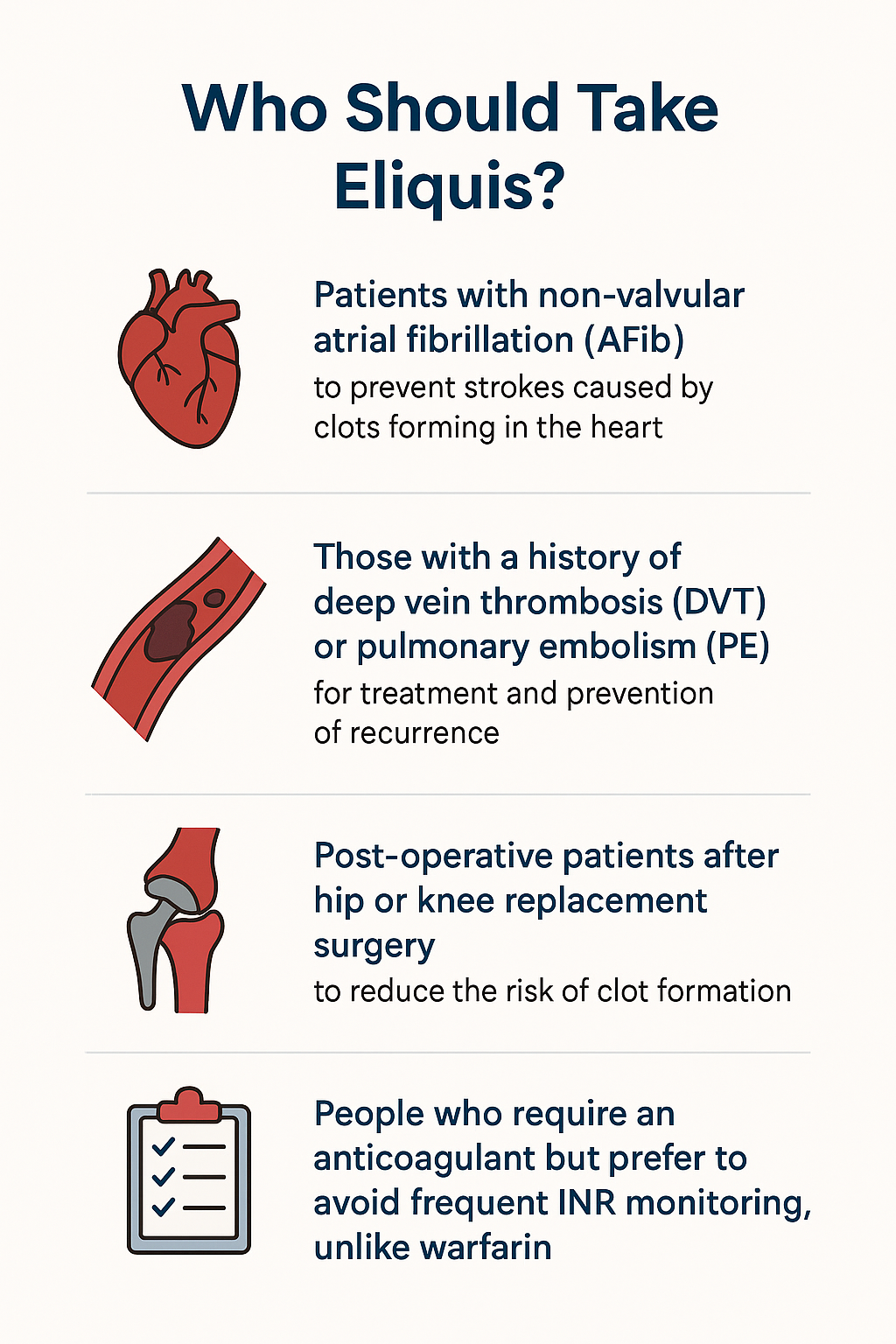
Patients with non-valvular atrial fibrillation (AFib): to prevent strokes caused by clots forming in the heart.
Those with a history of deep vein thrombosis (DVT) or pulmonary embolism (PE): for treatment and prevention of recurrence.
Post-operative patients after hip or knee replacement surgery: to reduce the risk of clot formation.
People who require an anticoagulant but prefer to avoid frequent INR monitoring, unlike warfarin.
Who Should Avoid Eliquis?
Eliquis is not suitable for individuals who:
Have active bleeding or a high risk of uncontrolled bleeding (e.g., recent hemorrhagic stroke).
Have severe hepatic impairment or coagulopathy-related liver disease.
Are taking strong dual inducers of CYP3A4 and P-glycoprotein (like rifampin), which reduce Eliquis’s effectiveness.
Are pregnant or breastfeeding, unless the benefits clearly outweigh risks (limited safety data).
Require mechanical heart valves or have moderate-to-severe mitral stenosis—Eliquis is not approved for these patients.
Doctors may adjust the dose or exercise caution in:
Elderly patients (age ≥80)
Those with low body weight (<60 kg)
People with renal impairment, especially if creatinine clearance is <30 mL/min
Always consult a healthcare provider before starting or stopping any anticoagulant.
Side Effects, Interactions, and Reversal
Like all medications, Eliquis (apixaban) carries the risk of side effects, though it is generally well-tolerated and considered safer than traditional anticoagulants like warfarin—especially in terms of major bleeding risks.
Common Side Effects
Minor bleeding: nosebleeds, bruising, gum bleeding
Gastrointestinal symptoms: nausea, indigestion
Anemia: in some long-term users due to chronic blood loss
Most mild side effects resolve on their own, but any unusual or prolonged bleeding should be evaluated by a healthcare provider.
Serious Side Effects
Major bleeding: especially in the gastrointestinal tract or brain
Hematuria: blood in urine
Hypotension and shock: in rare cases of internal bleeding
Unlike warfarin, Eliquis does not require routine INR monitoring, but patients should remain vigilant for any symptoms of serious bleeding, especially if taking it with other high-risk medications.
Drug Interactions
Eliquis is metabolized by the CYP3A4 enzyme and transported via P-glycoprotein (P-gp). Thus, several medications can affect its concentration:
Avoid or use with caution:
CYP3A4/P-gp inhibitors: ketoconazole, ritonavir (↑ bleeding risk)
CYP3A4/P-gp inducers: rifampin, carbamazepine (↓ effectiveness)
NSAIDs or antiplatelets: aspirin, clopidogrel (↑ bleeding risk)
Reversal Agent: Andexanet Alfa
In cases of life-threatening or uncontrolled bleeding, Andexanet alfa (Andexxa®) can rapidly reverse apixaban’s effects. This agent binds and neutralizes Factor Xa inhibitors, allowing clotting to resume normally.
Conclusion
Eliquis (apixaban) represents a major advancement in anticoagulant therapy, offering patients a safer, more convenient alternative to traditional blood thinners like warfarin. Its targeted mechanism—blocking Factor Xa—effectively reduces the risk of stroke, deep vein thrombosis, and pulmonary embolism, while minimizing the need for constant blood monitoring or strict dietary controls. With a well-established safety profile and a lower risk of serious bleeding events, Eliquis has become a preferred choice for patients with non-valvular atrial fibrillation and those recovering from orthopedic surgery.
However, as with any medication, it is essential for patients to be informed about potential side effects, drug interactions, and situations where its use may not be appropriate. Regular communication with healthcare providers, particularly regarding other medications or underlying health conditions, is crucial to ensure safe and effective use.
Whether you are a new patient starting Eliquis or someone researching options for clot prevention, understanding how this medication works can empower you to make confident, informed decisions about your treatment. Always consult your doctor before making any changes to your medication regimen.
Eliquis is a powerful tool in modern cardiovascular care—combining clinical efficacy with patient-friendly convenience.
References
Granger, C. B., Alexander, J. H., McMurray, J. J. V., Lopes, R. D., Hylek, E. M., Hanna, M., … & Wallentin, L. (2011). Apixaban versus warfarin in patients with atrial fibrillation. New England Journal of Medicine, 365(11), 981–992.
https://www.nejm.org/doi/full/10.1056/nejmoa1107039
Agnelli, G., Buller, H. R., Cohen, A., Curto, M., Gallus, A. S., Johnson, M., … & Weitz, J. I. (2013). Oral apixaban for the treatment of acute venous thromboembolism. New England Journal of Medicine, 369(9), 799–808.
https://www.nejm.org/doi/full/10.1056/NEJMoa1302507
Patel, M. R., Mahaffey, K. W., Garg, J., Pan, G., Singer, D. E., Hacke, W., … & Califf, R. M. (2011). Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. New England Journal of Medicine, 365(10), 883–891.
https://www.nejm.org/doi/full/10.1056/NEJMoa1009638
Heidbuchel, H., Verhamme, P., Alings, M., Antz, M., Diener, H. C., Hacke, W., … & Lip, G. Y. (2013). European Heart Rhythm Association practical guide on the use of new oral anticoagulants. Europace, 15(5), 625–651.
https://academic.oup.com/europace/article/15/5/625/675319
Connolly, S. J., Milling, T. J., Eikelboom, J. W., Gibson, C. M., Curnutte, J. T., Gold, A., … & Siegal, D. M. (2016). Andexanet alfa for acute major bleeding associated with factor Xa inhibitors. New England Journal of Medicine, 375(12), 1131–1141.
https://www.nejm.org/doi/full/10.1056/NEJMoa1607887
Mueck, W., Stampfuss, J., Kubitza, D., & Becka, M. (2014). Clinical pharmacokinetic and pharmacodynamic profile of rivaroxaban. Clinical Pharmacokinetics, 53(1), 1–16.




