Current Research about Metformin and Osteoarthritis
Abstract
In the extensive nationwide cohort study involving individuals with diabetes, the researchers found that treatment with metformin was associated with a significant reduction in the risk of developing osteoarthritis (OA) compared to sulfonylurea treatment. However, it is important to interpret these results with caution as we lacked data on body mass index (BMI), and it is possible that weight loss induced by metformin may have contributed to the observed benefit. Despite this limitation, the study adds to the growing body of evidence from preclinical and observational studies suggesting a potential protective association between metformin and OA development.
Osteoarthritis (OA) is a widespread condition that affects millions of people in the United States and is a significant contributor to global disability[1,2]. Despite current therapeutic approaches that mainly focus on managing symptoms, there is a significant unmet need for effective treatments that can halt, slow down, or reverse the progression of OA.
Metformin, a derivative of biguanide, is widely used as a first-line treatment for type 2 diabetes due to its ability to inhibit hepatic gluconeogenesis and increase muscle insulin sensitivity[3]. It is generally considered safe and affordable. In addition to its primary role in diabetes management, metformin has been associated with potential anti-inflammatory, anti-aging, anti-cancer, pro-weight loss, and immunomodulatory effects[4]. Recent evidence indicates that metformin may hold promise as a potential treatment or preventive measure for osteoarthritis (OA). Preclinical studies conducted in animal models, including mice, rats, and macaque monkeys, have revealed that metformin possesses disease-modifying properties in OA. Furthermore, observational studies conducted in humans have largely supported the use of metformin in preventing the development of OA or the need for joint replacement. However, many of these studies have primarily focused on the progression of preexisting OA and have not adequately accounted for the concurrent use of other anti-diabetic medications, thus limiting their ability to isolate the effects of metformin. Despite these limitations, the accumulating evidence suggests that metformin may hold promise as a potential therapeutic or preventive option for OA. Further research, including interventional studies, is warranted to better understand the efficacy and safety of metformin in OA treatment and prevention and to elucidate the underlying mechanisms of its beneficial effects[5]. Some studies have also suffered from immortal time bias related to the comparison of metformin users and nonusers, rather than using an active treatment control arm.
Based on the available preclinical and observational human data, there is a hypothesis that metformin use may prevent the development of OA. To further investigate this, researchers conducted a large-scale nationwide cohort study using time-conditional propensity score matching to assess the risk of developing OA and the need for joint replacement in individuals with diabetes who were treated with metformin compared to sulfonylurea, another class of anti-diabetic medication.
Primary Outcome
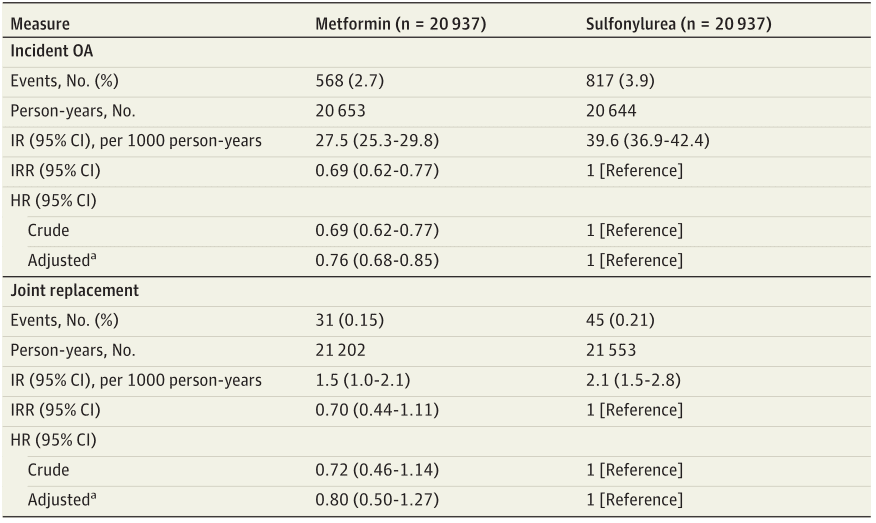
Using a robust prevalent new-user cohort design and employing time-conditional propensity score matching, our study found that individuals treated with metformin had a lower incidence rate (IR) of osteoarthritis (OA) at 27.5 events per 1000 person-years, compared to those treated with a sulfonylurea at 39.6 events per 1000 person-years, as indicated in Table 2[6]. After meticulous adjustment for potential confounders, including age, sex, race and ethnicity, geographical region, education, Charlson comorbidity score, and outpatient visit frequency, our results revealed that metformin treatment was associated with a significant 24% reduction in the likelihood of developing OA, as reflected by an adjusted hazard ratio (aHR) of 0.76 (95% CI, 0.68-0.85; P < .001), as presented in Table 2. These findings provide compelling evidence supporting the potential preventive effect of metformin in the development of OA, although further research is warranted. It is worth noting that our study has some limitations, including the lack of data on body mass index and the potential influence of metformin-induced weight loss on the observed results. Nevertheless, our findings contribute to the growing body of preclinical and observational data suggesting a protective association between metformin and OA and support the need for future interventional studies to investigate the role of metformin in OA treatment and prevention.
Table 2 Incidence and Risk of Developing OA and Undergoing Joint Replacement in Patients Treated With Metformin vs a Sulfonylurea
In the extensive nationwide cohort study involving individuals with diabetes, the researchers found that treatment with metformin was associated with a significant reduction in the risk of developing osteoarthritis (OA) compared to sulfonylurea treatment. However, it is important to interpret these results with caution as we lacked data on body mass index (BMI), and it is possible that weight loss induced by metformin may have contributed to the observed benefit. Despite this limitation, the study adds to the growing body of evidence from preclinical and observational studies suggesting a potential protective association between metformin and OA development. As a next step, future interventional studies should be considered to further investigate the role of metformin in the treatment or prevention of OA.
Strengths and Limitations
The study aimed to address some of the limitations of previous research by carefully accounting for concomitant medication use and utilizing a time-conditional propensity score matching approach, which helps to minimize potential biases. The researchers analyzed a large cohort of individuals with diabetes, comparing those treated with metformin to those treated with sulfonylurea, and assessed the development of OA and the need for joint replacement over time. By using propensity score matching, which helps to balance the characteristics of the study groups, the researchers aimed to create a more robust comparison.
The findings of this study have the potential to provide valuable insights into the role of metformin in the prevention of OA. If metformin is found to be effective in reducing the risk of developing OA or the need for joint replacement, it could represent a significant breakthrough in the field of OA management. With its established safety profile, affordability, and widespread availability, metformin could potentially offer a promising and accessible treatment option for OA prevention. Further research, including randomized controlled trials, will be needed to confirm the findings and establish metformin’s efficacy and safety for OA prevention. If proven effective, metformin could potentially fill the current gap in disease-modifying treatments for OA and offer hope for millions of people affected by this debilitating condition.