Antibody-Drug Conjugates Research and Applications
Abstract
Antibody-drug conjugates (ADCs) are a new class of highly potent oncology therapeutics for the treatment of people with cancer. They could be divided into three main structural units: the antibody; the cytotoxic agent (drug); and the linker. Discovery of ADCs bridged the gap between the cytotoxic drug and antibody, creating highly potent anticancer agents for targeted cancer therapy.
Introduction to Antibody-drug conjugates (ADCs)
Antibody-drug conjugates (ADCs) are a new class of highly potent oncology therapeutics for the treatment of people with cancer. They could be divided into three main structural units: the antibody; the cytotoxic agent (drug); and the linker. Discovery of ADCs bridged the gap between the cytotoxic drug and antibody, creating highly potent anticancer agents for targeted cancer therapy. Compared with other chemotherapeutic drugs, ADC drugs greatly improve the specificity of drug administration through the specific binding of antigens and antibodies. The antibody binds to the specific antigen on the tumor cell membrane to induce endocytosis, which enables the antibody and its attached cytotoxic small molecules to enter the cell and then be degraded by lysosomes. Small-molecule drugs are released into cells and induce apoptosis through DNA insertion or inhibition of microtubule synthesis. The concept of ADC has been proposed for more than 100 years. However, due to the difficulty in development, most of the drugs under development are still in the early stage of research, and few ADC drugs can be successfully marketed. There has been a significant increase in the number of clinical trials with anticancer ADCs and the following is a list of ADCs in clinical trials.
BCMA
Human multiple myeloma (MM) is a malignant plasma cell tumor. It has been found that B cell maturation antigen (BCMA) is commonly expressed on the surface of MM cells. GSK2857916 is a novel humanized and fucosylated anti-BCMA antibody-drug conjugate via a non-cleavable linker. GSK2857916 blocked cell growth through the G2/M phase, induced Caspase-3-dependent apoptosis of myeloma cells, and was co-cultured with bone marrow stromal cells or various effector cells. It strongly inhibits the colony formation of MM cells without affecting BCMA-negative normal cells. The results show that GSK2857916 has effective and selective anti-MM activity through a variety of cytotoxic mechanisms, providing a promising new generation of immunotherapy for the treatment of this cancer. The molecule is currently in phase 1 clinical study, and more data are still being studied.
CD19
CD19 antigen is a type I transmembrane glycoprotein belonging to the immunoglobulin Ig superfamily. CD19 was specifically expressed in both normal and tumor B cells. The expression pattern of CD19 remains unchanged in B-cell malignancies, and it is expressed in the inert and aggressive subtypes of NHL, B-cell CLL, and non-T acute lymphoblastic leukemia. SAR3419(huB4-DM4) is a new type of ADC that is composed of a humanized monoclonal IgG1 anti-CD19 antibody (huB4) attached to the potent cytotoxic drug, a maytansine derivative (N2′-deacetyl-N2′-[4-mercapto-4-methyl-1-oxopentyl] [DM4]), through a cleavable disulfide cross-linking agent, N-Succinimidyl-4-2-pyridyldithio butanoic acid (SPDB). SAR3419 has been approved for phase 2 clinical trials. Denintuzumab mafodotin (SGN-CD19A) is a CD19-targeting antibody-drug conjugate, comprising a monoclonal antibody conjugated to the potent cytotoxin monomethyl auristatin F. Since SGN-CD19A has previously shown activity against B-cell malignancies in early-stage clinical trials, it was of interest to test it against the Pediatric Preclinical Testing Program preclinical models of CD19+ pediatric acute lymphoblastic leukemia (ALL). The Phase 1 clinical trial of SGN-CD19A is well underway.
CD22
CD22 is an antigen with expression limited to B cells and the vast majority of non-Hodgkin lymphomas (NHL). CD22 is a 130 kDa type I transmembrane glycoprotein, normally expressed on B-lineage cells from the pre-B-cell stage and is also expressed on most malignant mature B cells, including follicular NHL, marginal zone lymphoma (MZL), MCL, DLBCL, small lymphocytic lymphoma (SLL), and CLL. DCDT2980S which is in phase I clinical heist consists of a humanized anti-CD22 monoclonal IgG1 antibody with a potent microtubule-disrupting agent, monomethyl auristatin E (MMAE), linked to the reduced cysteines of the antibody via a protease cleavable linker, maleimidocaproyl-valine-citrulline-p-aminobenzoyloxycarbonyl (MC-vc-PAB). Inotuzumab ozogamicin(CMC-544) is a CD22 monoclonal antibody bound to calicheamicin, a natural product of Micromonospora echinospora, which is significantly more toxic than cytotoxic chemotherapy.1Inotuzumab binds CD22 with subnanomolar affinity and is rapidly internalized, delivering the conjugated calicheamicin intracellularly. At present, the phase III clinical study is in progress.
CD27L
CD27L, also known as CD70 or TNFSF7, is a type II integral membrane protein expressed on a subset of activated T cells, B cells, and mature dendritic cells. The receptor for this ligand, CD27, is expressed in a large proportion of natural killer cells and most resting T cells and B cells. AMG 172 is an antibody-drug conjugate (ADC) comprised of anti–CD27L-MCC-DM1, where anti-CD27L is a fully human immunoglobulin (Ig) G1 monoclonal antibody, MCC is the non-cleavable linker 4-[N-maleimidomethyl] cyclohexane-1-carboxylate conjugated to lysine residues in the antibody, and DM1 is a semisynthetic derivative of the ansamycin antibiotic, maytansine, conjugated to MCC. SGN-75, an auristatin-based anti-CD70 ADC, recently entered a phase I clinical trial for patients with renal cell carcinoma and NHL. The ADC drugs are currently in clinical trials with tumor reductions and minimal toxicity observed. The clinical potential of empowered antibodies has heightened the pursuit of ADCs for additional targets and tumor indications.
CD30
CD30 is an attractive target for monoclonal antibody therapy because of its limited expression on normal tissues and its uniform, high-level expression on malignant cells in patients with classical Hodgkin lymphoma and anaplastic large-cell lymphoma. Brentuximab vedotin (SGN-35) is an antibody-drug conjugate (ADC) directed against the CD30 antigen expressed in Hodgkin lymphoma and anaplastic large-cell lymphoma. SGN-35 consists of the cAC10 chimeric IgG1 monoclonal antibody SGN30, modified by the addition of a valine-citrulline dipeptide linker to permit attachment of the potent inhibitor of microtubule polymerization monomethyl auristatin E (MMAE). Targeted binding of SGN-35 increases apoptosis in CD30-positive tumor cells. This is especially important in ALCL, where most of the cells within the tumor mass are CD30-positive cells and delivery of an apoptotic signal is expected. CD30 monoclonal antibodies may induce proliferation, as described in Hodgkin lymphoma cell lines, and the delivery of MMAE in the context of a proliferative signal may enhance apoptosis. Second, once it is liberated from the monoclonal antibody, free MMAE can diffuse from the cell into the surrounding stroma, resulting in a bystander effect. This has special relevance for Hodgkin lymphoma, in which the inflammatory and immune cells that make up most of the tumor mass provide growth factor support and help the malignant HRS cells avoid immune recognition. Now, Brentuximab vedotin has been approved by the FDA.
CD33
CD33 is a myeloid cell differentiation antigen with a molecular weight of 67KD, which is mainly distributed in myeloid blood cells, especially in the early stage of differentiation. CD33 is expressed in more than 90% of patients with acute myeloid leukemia. CD33 is not expressed on the surface of hematopoietic stem cells, nor in mature granulocytes or other tissues, making it a good target for the treatment of myeloid leukemia. SGN-CD33A which is currently in a Phase I clinical study consists of an anti-CD33 mAb conjugated to a novel synthetic pyrrolobenzodiazepine (PBD) dimer structurally related to anthramycin isolated from Streptomyces refuineus. Molecules in the PBD family cause cell death by crosslinking DNA and interrupting cell division and are being explored clinically for the treatment of human cancer. Studies demonstrate that SGN-CD33A has robust activity in vitro against a broad panel of AML cell lines and primary patient samples. Gemtuzumab ozogamicin is a humanised monoclonal IgG4 antibody, linked to a cytotoxic calicheamicin derivative. It effects cell necrosis by specifically targeting the CD33 antigen. Gemtuzumab ozogamicin has been approved for use in the US for the treatment of CD33+ AML in patients aged ≥60 years who are in first relapse and who are not considered candidates for other cytotoxic chemotherapy. Gemtuzumab ozogamicin has shown clinical efficacy in this indication and is relatively well tolerated.
CD56
CD56 is a group of related cell surface glycoproteins that play an important role in embryogenesis and development as well as in the interconnectedness of nerve cells. It has been reported that CD56-positive cancers are more aggressive than CD56-negative cancers. The CD56 antigen is mainly expressed in neurons, astrocytes, Schwann cells, NK cells, and a small number of activated T lymphocytes. This antibody is expressed in lung small cell carcinoma, mesothelioma, carcinoid, islet cell tumor, pancreatic tumor with neuroendocrine differentiation, and other malignant tumors. Lorvotuzumab mertansine (LM) is an ADC composed of an anti-CD56 humanized N901 monoclonal antibody conjugated via a stable disulfide linker to the maytansinoid DM1. Once bound to CD56 on the surface of the target cell the conjugate is internalized, the linker is cleaved, and DM1 is released which in turn inhibits tubulin polymerization and results in cell death. Maytansine is clinically active but its narrow therapeutic window precluded further clinical development. Conjugation to an antibody and intracellular delivery could take advantage of the cytotoxic potency and expand the therapeutic window leading to greater tumor cell death with less overall toxicity. The maytansine derivative DM1 was developed specifically for use in ADCs.
CD37
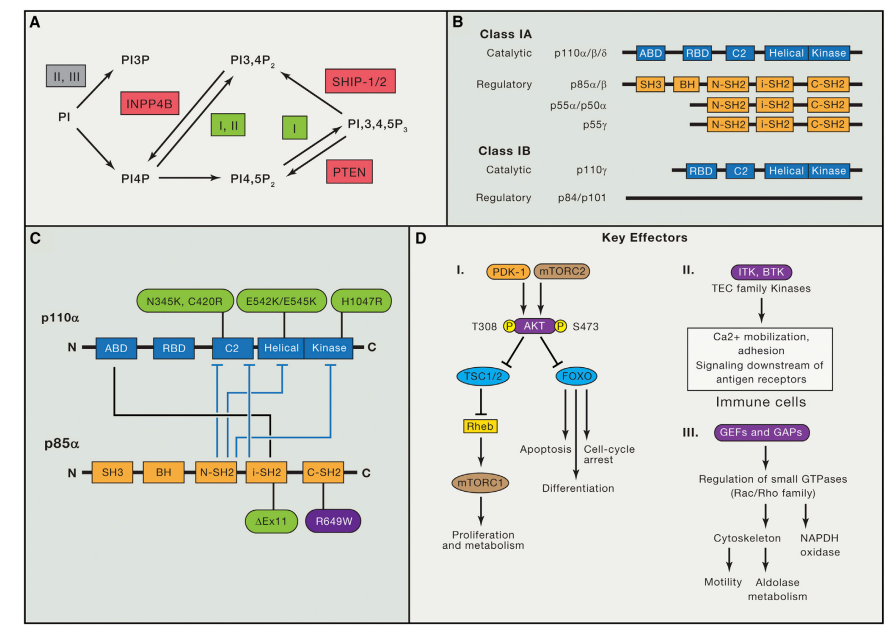
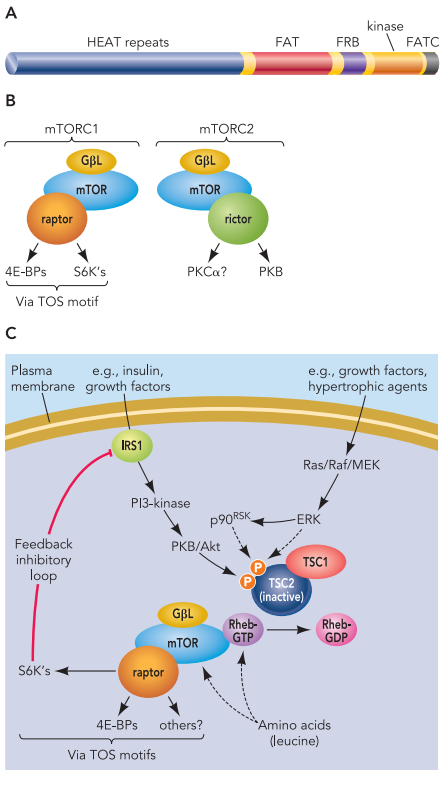
CD37 is a tetraspanin protein highly expressed on malignant B-cells in CLL and non-Hodgkin lymphoma. Although a natural ligand for CD37 remains unknown, signaling induced by the anti-CD37 peptide SMIP-016 has implicated this tetraspanin as a mediator of the PI3K (phosphatidylinositol 30-kinase)/Akt survival pathway. Through cytoplasmic immunoreceptor tyrosine-based activating motif and immunoreceptor tyrosine-based inhibition-like motifs with opposing functions, CD37 can directly participate in both prosurvival and pro-apoptotic signaling by facilitating alterations in the phosphorylation state of Akt. IMGN529 is an antibody–drug conjugate (ADC) in which the cytotoxic maytansine-derivative DM1 is linked to a CD37-targeting humanized IgG1 antibody via a stable SMCC linker. This strategy seeks to combine the potent cytotoxicity demonstrated by anti-CD37 therapeutics with the specific delivery of DM1, which exerts anti-proliferative effects by disrupting microtubule dynamics during mitosis. AGS 67E is a novel ADC drug which consists of a fully human IgG2 antibody targeting CD37 conjugated to the anti-tubulin agent monomethyl auristatin E via a cleavable linker for potential therapy of lymphoid malignancies. Both drugs are currently in Phase I clinical studies.
CD74
CD74 is a type II transmembrane glycoprotein of 216 amino acids, which associates with the MHC class II a and h chains and directs the transport of class II molecules to lysosomal and endosomal compartments, where the invariant chain is degraded. CD74 was shown recently to bind to a cytokine, macrophage migration inhibitory factor, and to play a role in macrophage migration inhibitory factor-induced activation of signaling events. In current studies, it showed excellent therapeutic efficacy of IMMU-110 in a xenograft model of human B-cell lymphoma, affecting cures of severe combined immunodeficient (SCID) mice given previously a lethal i.v. injection of Raji lymphoma cells. The high prevalence of CD74 antigen expression in multiple myeloma clinical specimens, together with a frequently developed resistance to anthracyclines, prompted researchers to perform a comprehensive clinical evaluation of IMMU-110 conjugate in a new multiple myeloma xenograft model. Milatuzumab doxorubicin is a conjugate of milatuzumab (humanized monoclonal antibody targeting tumors expressing CD74 antigen) with doxorubicin. These two drugs for the treatment of Multiple myeloma(MM) are undergoing phase I/Ⅱ clinical efficacy evaluation.
CD66e
Carcinoembryonic antigen (CEA), also known as CD66e and CEACAM5, is a glycoprotein with a molecular weight of 180-200kD involved in cell adhesion. CEA is usually produced in the fetal digestive system, but because it is suppressed after birth, normal adults usually have very low levels of CEA in their colon and blood. However, CEA in serum levels can be made including colorectal cancer, lung cancer and breast cancer, bow | up several types of cancer. CEA is therefore widely used as a broad-spectrum tumor marker. CEA is not specific for any type of cancer, but the concentration of CEA in blood can predict the therapeutic effect, progression and prognosis of cancer. Labetuzumab govitecan (IMMU130) is an ADC that uses a proprietary linker to site-specifically couple SN-38 to labetuzumab. Labetuzumab is a slowly internalizing humanized antibody whose clinical safety and antitumor activity as a radioconjugate have been reported. This agent targets CEACAM5 (CD66e) antigen expressed on many solid cancers.
CD79b
CD79 is a heterodimer molecule involved in signal transduction as a component of the B cell receptor (BCR). Cd79 is composed of two peptide chains, CD79a and CD79b (Igα and Igβ, respectively). It is highly specific to B cell lineage and highly expressed in a variety of B cell NHL and chronic lymphocytic leukemia B cells. It has the mechanism of action of killing B cell tumors extensively. At the same time, preclinical studies have also verified that CD79b as a binding site is more efficient than targeting CD79a. Therefore, CD79b becomes an ideal therapeutic target to play the action mechanism of ADC, which can effectively deliver payload drugs and cause targeted cytotoxic killing through exquisite endocytosis and transfer to lysosomal-like loci rich in proteases. Polatuzumab vedotin(RG7596) is an antibody-drug conjugate consisting of the microtubule-disrupting agent monomethyl auristatin E (MMAE) conjugated to an anti-CD79B monoclonal antibody by the protease-cleavable peptide linker maleimidocaproylvaline-citrulline-paminobenzoyloxycarbonyl. Its clinical trials are still underway.
CD138, Syndecan1
CD138, also known as syndecan-1, located in chromosome 2p23-24, is a transmembrane glycoprotein, mainly involved in the regulation of cell growth and differentiation, cell adhesion, and migration. It is expressed in preB cells and plasma cells, but not in mature B cells. It can be used in the differential diagnosis of lymphoplasmacytic lymphoma (+) and marginal zone lymphoma (-). CD138 is primarily used to label normal plasma cells and their tumors. It is an important marker for multiple myeloma and is also expressed in normal epithelium. Indatuximab ravtansine (BT062) is in phase II clinical study and is an antibody-drug conjugate (ADC) consisting of the anti-CD138 chimeric monoclonal antibody (nBT062) and the microtubule-binding cytotoxic agent maytansinoid DM4. Indatuximab ravtansine specifically targets CD138-expressing cells; once internalized, lysosomal processing of its linker results in the release of DM4, which in turn binds to tubulin and causes cell cycle arrest followed by apoptotic cell death.
CA6
Due to the abnormal expression of MUC1(CA6) in tumor tissues, MUC1 has become an important biomarker of tumor. MUC1 is widely distributed and abnormally abundant expressed on the surface of cancer cells. Due to incomplete glycosylation, it exposes the normally concealed epitopes and becomes the attack target of immune cells. SAR566658 (huDS6-SPDB-DM4). This product is an ADC consisting of the humanized monoclonal antibody (mAb) huDS6 conjugated to DM4, a potent cytotoxic maytansinoid derivative which inhibits tubulin polymerization, recognizing a tumor-associated sialoglycotope on CA6 in solid tumors. In a Phase I trial of 114 patients, tumor regression was seen in 60% of patients given 190 and 90 mg/m2 doses on day 1 and day 8; In the 150 and 120 mg/m2 fortnightly dosing groups, 35% of patients experienced tumor regression.
CAIX
Carbonic anhydrase IX (CAIX) is a cell surface glycoprotein that is expressed in many different tumors and yet restricted in normal tissues to the gastrointestinal tract. It is upregulated by hypoxia and correlates with tumor grade and poor survival in several tumor indications. Through the selection process, the 3ee9 mAb was identified, which upon conjugation to monomethyl auristatin E through a self-immolated enzyme-cleavable linker yielded the potent and selective CAIX antibody-drug conjugate CAIX-ADC (BAY79-4620). In preclinical human xenograft models in mice representing several tumor indications, BAY79-4620 showed potent antitumor efficacy, and some models showed partial and complete tumor shrinkage even following a single dose. The phaseⅠclinical data collectively support the development of BAY79-4620 for the treatment of cancer patients with CAIX overexpressing Tumors.
CanAg
CanAg is a sialic carbohydrate antigen that can be recognized by Ca242, one of a series of monoclonal antibodies obtained by the hybridoma technique in colon cancer cell lines. It is a mucin-type glycoprotein present in multi-organ malignancies, that is, does not react with LewisA-type antigen, nor does it react with sialic galactoside. Immunochemical studies have shown that it is different from other known tumor-associated mucins such as Ca199, Ca50, Ca125, Ca153, etc., and its content is low in the serum of healthy people and with benign diseases. CanAg is a relatively new tumor marker applied in the clinic in recent years, which is a good tumor marker for pancreatic cancer and colon cancer. IMGN242 is under phase Ⅰ clinical trial and is a conjugate of the cytotoxic maytansinoid DM4 and the monoclonal antibody huC242, which binds to CanAg.
C-Kit
C-Kit (CD117) is a type III receptor tyrosine kinase that binds stem cell factors. When this receptor binds to a stem cell factor, it forms a dimer that activates its intrinsic tyrosine kinase activity, reversely phosphorylates it and activates signal transduction molecules. In recent years, it has been found that c-kit gene mutations, especially active mutations, are closely related to the pathogenesis, treatment, and prognosis of acute leukemia. The monoclonal antibody moiety of anti-C-Kit ADC LOP628 targets and binds to the cell surface antigen c-Kit. After antibody-antigen interaction followed by internalization, the maytansine moiety binds to tubulin, inhibits microtubule assembly, and induces microtubule disassembly. This leads to a disruption of mitosis and the inhibition of cell proliferation in cancer cells expressing c-Kit. Yet the clinical trial has been terminated in 2019.
EGFR
Glioblastoma (GBM) is the highest grade glioma and is the most common malignant primary brain tumor in adults. Despite available treatment options, most patients with the recurrent disease survive < 1 year. The epidermal growth factor receptor (EGFR) gene has been reported to be highly amplified in a substantial proportion of primary and recurrent GBM, and approximately 50% of such tumors have a mutation in which exons 2–7 is deleted, resulting in a splice variant between exons 1 and 8, termed “EGFR variant III” (EGFRvIII). AMG 595 is an antibody-drug conjugate comprising a fully human, anti-EGFRvIII monoclonal antibody linked to the maytansinoid DM1, a semisynthetic derivative of maytansine. AMG 595 binds to EGFRvIII but not native EGFR; after binding, the AMG 595–EGFRvIII complex is internalized via the lysosomal pathway, leading to the release of DM1 and mitotic arrest. The phase I clinical trial for Glioblastoma, Advanced malignant glioma, anaplastic astrocytomas, and glioblastoma multiforme is ongoing now. IMGN289 is a novel ADC consisting of the humanized anti-EGFR antibody, J2898A, covalently linked to the potent cytotoxic maytansinoid, DM1. IMGN289 can inhibit the proliferation of nasopharyngeal carcinoma cells by reducing their clonicity, and it also shows certain inhibitory activity in other monoclonal resistant cells.
Cripto-1
Cripto is a GPI-linked protein required for signal transduction of the TGF-beta ligand, Nodal. Cripto has been previously described as an oncogene and fits the classic pattern of an embryonic gene that is re-expressed in a transformed tumour cell. Cripto expression is highly prevalent on a number of solid tumours, including greater than 75% of breast, lung, and colorectal tumours. Developmental data suggest that the Cripto–Nodal pathway plays a role in determining mesenchymal cell fate. BIIB015 is an immunoconjugate created for the treatment of solid tumours and is currently in Phase I of clinical evaluation. BIIB015 consists of a humanised monoclonal antibody against the Cripto protein carrying a payload, via a hindered disulphide linker, of the maytansinoid derivative, DM4.
ENPP3
ENPP3 is an ectonucleotide pyrophosphatase/phosphodiesterase protein with high expression in some tumors such as clear cell renal cell carcinoma and generally low expression in normal tissues. AGS-16C3F is an ADC currently being investigated in a Phase II study in metastatic renal cell carcinoma (mRCC). AGS-16C3F is comprised of a fully human IgG2 monoclonal ENPP3-targeting antibody conjugated to monomethyl auristatin F (MMAF) via a non-cleavable maleimidocaproyl linker. For the Phase I clinical trial with AGS-16C3F, thrombocytopenia was observed in 11 of 34 patients. Of these 11, 6 subjects (18%) experienced Grade 3 or 4 events with no obvious clinical implications.
GPNMB
Glycoprotein NMB (GPNMB), or osteoactivin, is a transmembrane glycoprotein primarily expressed in intracellular compartments (e.g., lysosomes and melanosomes) in the non-malignant cell such as melanocytes, osteoclasts, and osteoblasts. In hepatocellular carcinoma, breast cancer, glioblastoma, and melanoma, membrane GPNMP is overexpressed, making it a reasonable candidate for targeted therapeutics. Glembatumumab vedotin is an antibody-drug conjugate (ADC) currently being investigated in a Phase I study that combines an anti-GPNMB antibody with the anti-mitotic agent monomethyl auristatin E (vedotin). Glembatumumab vedotin showed in vitro cytotoxicity that was related to GPNMB expression, and it induced complete regressions in GPNMB-expressing melanoma and breast cancer xenografts.
Guanylyl cyclase C
GCC(guanylyl cyclase C) is a member of the guanylyl cyclase (GC) family of proteins which includes at least seven forms, A through G. Endogenous ligands, however, have been identified only for forms A, B, and C. GCs are involved in the regulation of intracellular cGMP concentrations. On the other hand, GCC is a tumor suppressor and it is regulated by caudal type homeobox transcription factor-2 (CDX-2) and it prevents cancer cell proliferation. A novel ADC, MLN0264 (TAK-264) is an anti-guanylyl cyclase C antibody conjugated via a protease-cleavable linker to the potent anti-microtubule agent monomethyl auristatin E (MMAE) (linker and toxin licensed from Seattle Genetics). Following binding to GCC, the ADC is internalized and transported to lysosomes where MMAE is released to bind to tubulin, leading to cell cycle arrest and apoptosis. This GCC targeting ADC has been evaluated in clinical studies in patients with advanced gastrointestinal malignancies.
Her2
Amplification of human epidermal growth factor receptor 2 (HER2, also called ErbB2) occurs in approximately 20% of breast cancers and is associated with shortened survival. Combining HER2-targeted agents with standard chemotherapy is an effective therapeutic approach for patients with HER2-positive metastatic breast cancer. The current effective treatment for HER2-positive metastatic breast cancer is targeted drugs combined with standard chemotherapy. Trastuzumab emtansine (T-DM1) is an antibody-drug conjugate that combines a HER2-antigen-targeting trastuzumab with a cytotoxic microtubule inhibitor DM1 via a stable linker. T-DM1 allows intracellular drug molecules to target cells that overexpress HER2, reducing the impact on normal tissue. T-DM1 was first approved by the FDA in 2013 as a single agent for the treatment of patients with HER2-positive metastatic breast cancer.
LIV-1
LIV-1 is a member of the solute carrier family 39; a multi-span transmembrane protein with putative zinc transporter and metalloproteinase activity. It was first identified as an estrogen-induced gene in the breast cancer cell line ZR-75-1. LIV-1 expression has been linked to epidermal-to-mesenchymal transition (EMT) in both normal vertebrate embryo development and preclinical models leading to malignant progression and metastasis. There is evidence of LIV-1 interacting with the transcription factors STAT3 and Snail to down-regulate expression of E-cadherin to promote EMT. SGN-LIV1A consists of a humanized antibody conjugated through a proteolytically cleavable linker to monomethylauristatin E, a potent microtubule-disrupting agent. When bound to surface-expressed LIV-1 on immortalized cell lines, this ADC is internalized and traffics to the lysozome. SGN-LIV1A displays specific in vitro cytotoxic activity against LIV-1 expressing cancer cells.
Mesothelin
Mesothelin is a tumor differentiation antigen frequently overexpressed in tumors such as mesothelioma, ovarian, pancreatic, and lung adenocarcinomas while showing limited expression in nonmalignant tissues. Mesothelin is therefore an attractive target for cancer therapy using antibody-drug conjugates (ADC). Anetumab ravtansine(BAY 94-9343) which is currently in phase I clinical trials is a novel ADC consisting of a human anti-mesothelin antibody conjugated to the maytansinoid tubulin inhibitor DM4 via a disulfide-containing linker. Effects of BAY 94-9343 on cell proliferation were first studied in vitro and subsequently in vivo using subcutaneous, orthotopic, and patient-derived xenograft tumor models. The antibody binds to human mesothelin with high affinity and selectivity, thereby inducing efficient antigen internalization. In vitro, BAY 94-9343 demonstrated potent and selective cytotoxicity of mesothelin-expressing cells with an IC50 of 0.72 nmol/L, without affecting mesothelin-negative or nonproliferating cells. In vivo, BAY 94-9343 localized specifically to mesothelin-positive tumors and inhibited tumor growth in both subcutaneous and orthotopic xenograft models.
Nectin-4
Nectin-4 (PVRL4), a type I transmembrane protein and member of a family of related immunoglobulin-like adhesion molecules, is a potential target in epithelial cancers. Nectin-4 is a member of the nectin family of immunoglobulin (Ig)-mediate Ca2+-independent cell-cell adhesion via both homophilic and heterophilic trans-interactions at adherens junctions, where they recruit cadherins and modulate cytoskeleton rearrangements. A novel antibody-drug conjugate (ADC) enfortumab vedotin comprising the human anti-nectin-4 antibody conjugated to the highly potent microtubule disrupting agent MMAE. Hybridoma (AGS-22M6E) and CHO (ASG-22CE) versions of enfortumab vedotin (also known as ASG-22ME) ADC were able to bind to cell surface expressed nectin-4 with high affinity and induced cell death in vitro in a dose-dependent manner. Treatment of mouse xenograft models of human breast, bladder, pancreatic, and lung cancers with enfortumab vedotin significantly inhibited the growth of all four tumor types and resulted in tumor regression of breast and bladder xenografts.
PMSA
Prostate-specific membrane antigen (PSMA) is a membrane protein that is overexpressed in manifold in prostate cancer and provides an attractive target for therapy. PSMA is expressed in nearly all prostate cancers, and expression is highest in poorly differentiated, metastatic, and hormone-refractory cases. PSMA also is expressed in a variety of tumors, but not normal, vascular endothelium, which further broadens its potential utility as a therapeutic target. The cytoplasmic tail of PSMA mediates its internalization both in the presence and absence of mAbs. With its abundant and restricted expression in tumors, its membrane location, and rapid internalization, PSMA has characteristics desired in a target for ADC therapy. PSMA ADC is an antibody-drug conjugate (ADC) that consists of a fully human anti-PSMA monoclonal antibody conjugated to monomethylauristatin E through a valine-citrulline linker. Anti-PSMA monoclonal antibodies (mAbs) have also been developed as bioligands for diagnostic imaging and targeted PC therapy. However, these mAbs are successfully used in PC imaging and only a few have gone beyond phase-I for targeted therapy. Here are some studies that showed anti-PSMA ADC can successfully control the growth of PSMA(+) tumors without inducing systemic toxicity.
SLC44A4
SLC44A4, also known as CTL4, is a member of the family of solute carrier proteins known as SLC44A1-5 or choline transporter-like proteins (CTL1-5). SLC44A4 has not been shown to be involved in choline transport but it has been linked with acetylcholine synthesis and transport as well as uptake of thiamine pyrophosphate, the phosphorylated form of vitamin B1. SLC44A4 is normally expressed on the apical surface of secretory epithelial cells but in cancer, we show expression is not restricted to the luminal surface in advanced and undifferentiated tumors. ASG-5ME which is currently in phase I clinical trials consists of a human IgG2 anti-SLC44A4 antibody conjugated through a cleavable linker to the microtubule-disrupting agent, monomethylauristatin E. It has potent anti-tumor activity in both cell line and patient-derived xenograft models of pancreatic and prostate cancers.
SLITRK6
SLITRK6 was discovered as a bladder tumor antigen which is a member of the SLITRK family of proteins. The SLITRK family members are type I transmembrane proteins that share conserved leucine-rich repeat domains similar to those in the secreted axonal guidance molecule, SLIT. SLITRK6 is expressed at high levels in bladder cancer and to a lesser extent in other epithelial tumors (lung, breast, and glioblastoma). ASG-15ME (Product name, AGS15E) is composed of a SLITRK6specific human gamma 2 antibody (Igγ2) conjugated to MMAE via a protease-cleavable linker. The studies confirmed that ASG-15ME is rapidly internalized after binding to cell surface SLITRK6. ASG-15ME is currently in Phase I Clinical Trials for the treatment of metastatic urothelial cancer.
Tissue factor
Tissue factor(TF), also called thromboplastin, factor III, or CD142 is aberrantly expressed in many types of cancers, including non–small cell lung cancer, colorectal cancer, genito-urethal, and gynecologic cancers, pancreatic cancer, head and neck cancer, glioma, and metastatic breast cancer. The specific TF antibody that interferes with TF: is FVIIa-dependent intracellular signaling, but not with the procoagulant activity of TF. TF-011-MMAE(HuMax-TF-ADC) was designed to specifically target tumor cells that aberrantly express TF, without interfering with the role of TF in coagulation. TF-011-MMAE showed potent antitumor activity in xenograft models derived from a broad range of solid cancers, and an acceptable safety profile in nonclinical toxicity studies.
TROP-2
TROP-2 is encoded by a single-copy gene (TACSTD2) mapped on chromosome 1p32. First described as a cell-surface glycoprotein of a human trophoblast cell, Trop-2 was believed at that time to be involved in regulating the growth and invasion of cancer cells. Functionally, it is linked to cell migration and anchorage-independent growth, with higher expression in a variety of human epithelial cancers, including breast, lung, gastric, colorectal, pancreatic, prostatic, cervical, head-and-neck, and ovarian carcinomas, compared to normal tissues. IMMU-132 which is currently in phase II clinical trials, is important because it represents a significant departure from the current ADC paradigm of using a stably-linked ultratoxic drug by: (i) use of a moderatelytoxic drug, SN-38, (ii) conjugation of drug to monoclonal antibody (mAb) at a high ratio (~8:1) without affecting antibody targeting and pharmacokinetics, (iii) utilization of a pH-sensitive, cleavable linker designed to impart cytotoxic activity to both target and bystander cells via ADC internalization and local release of the free drug at the tumor, (iv) allowing high doses of the ADC over a prolonged times without provoking an immune response, and (v) showing reduced toxicities, especially a lower incidence of severe diarrhea, which is common for topoisomerase inhibitors.