Alopecia Areata Advances: New Treatments, Tools, and Insights You Need to Know
Abstract
This article explores the most recent advances in Alopecia Areata (AA) research from 2023 to 2025, covering new treatment strategies, diagnostic tools, psychological impacts, and demographic-specific considerations. It highlights the role of JAK inhibitors such as baricitinib and tofacitinib in transforming care, as well as the use of dermoscopy and genetic insights for early diagnosis. Special focus is given to pediatric and gender-specific issues and the integration of mental health into treatment planning. The post concludes with a forward-looking perspective on precision medicine and equitable access. This article provides a concise, evidence-based overview for patients, dermatologists, and healthcare professionals seeking up-to-date knowledge on AA.
Introduction: Why Alopecia Areata Research Matters
Alopecia Areata (AA) is more than just hair loss—it’s a complex autoimmune condition that disrupts the immune system’s interaction with hair follicles, often resulting in sudden and unpredictable hair shedding. Affecting nearly 1 in 100 people globally, this condition can emerge at any age and manifest in varying degrees—from small bald patches to complete hair loss across the scalp or body.
While alopecia is not life-threatening, its psychological burden is substantial. Many individuals report anxiety, depression, social withdrawal, and lowered self-esteem—particularly when hair loss is visible or occurs during formative years. Because of this emotional impact, AA is not just a dermatological issue but also a mental health and quality-of-life concern.
Over the last decade, the understanding of AA’s molecular and immunological basis has grown rapidly. Previously limited to topical corticosteroids and unpredictable regrowth, AA treatment has now entered a transformational era with the emergence of targeted therapies like JAK inhibitors, which aim to reset immune dysfunction at the follicular level. In parallel, new tools for diagnosis, genetic profiling, and patient-reported outcomes are reshaping how clinicians approach this condition.
As research continues to uncover the mechanisms, predictors, and psychosocial dimensions of AA, it’s vital for clinicians, patients, and caregivers to stay informed. The latest scientific findings not only offer hope for lasting treatments but also foster a more empathetic and personalized standard of care.
Breakthrough Treatments — JAK Inhibitors and Beyond
The treatment landscape for Alopecia Areata (AA) has undergone a dramatic transformation in recent years. Once dominated by corticosteroids and immunotherapies with mixed results, modern research has introduced targeted molecular treatments, particularly Janus kinase (JAK) inhibitors, as game-changers in severe AA.
Among these, baricitinib became the first JAK inhibitor to receive FDA approval in 2022 for the treatment of severe alopecia areata. It works by blocking the overactive immune signals—specifically the JAK-STAT pathway—that lead to follicular inflammation and hair loss. Recent pediatric case reports have shown remarkable regrowth with baricitinib, suggesting its potential across age groups.
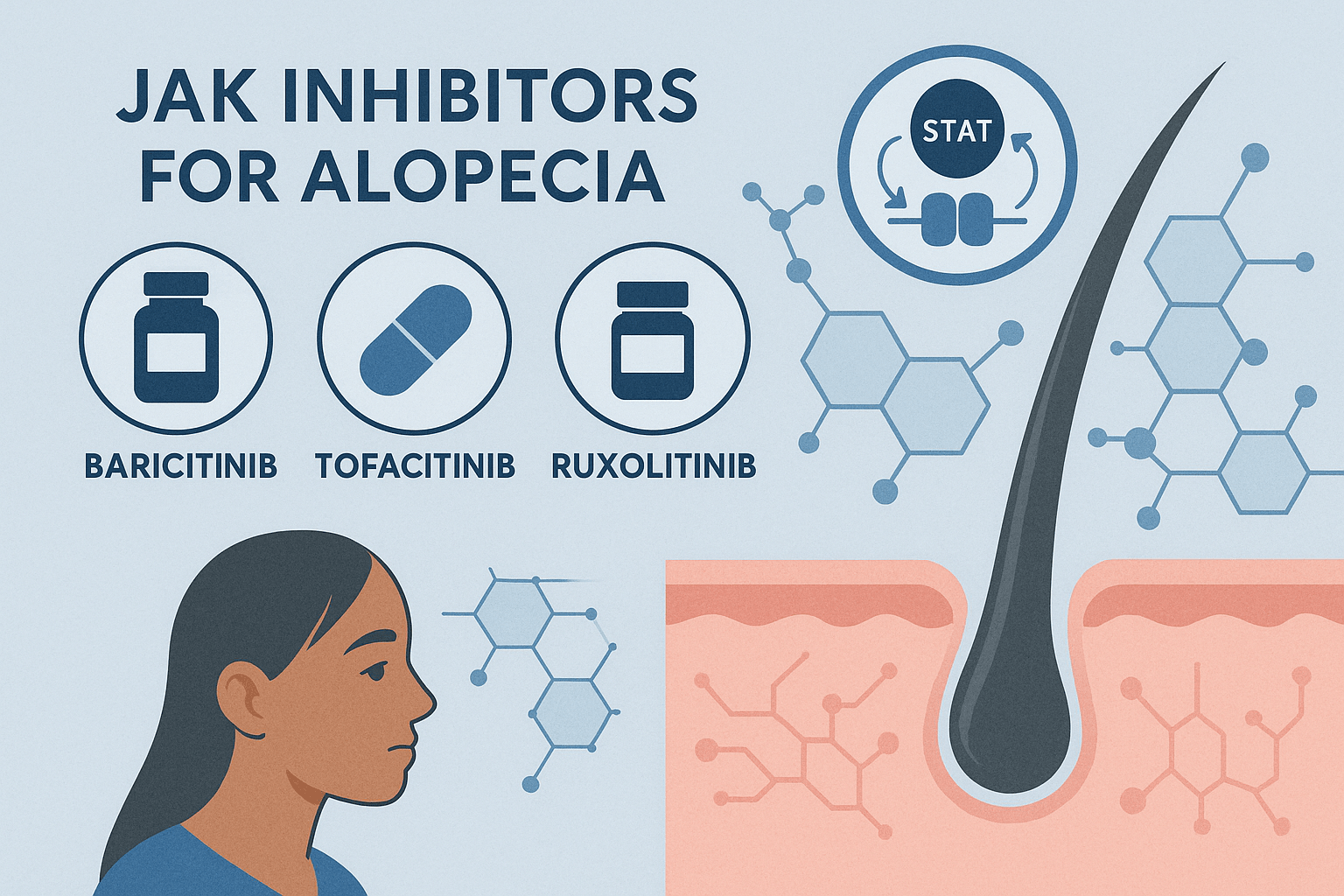
Other JAK inhibitors, such as ruxolitinib and tofacitinib, have also shown promise in both clinical trials and real-world use. A 2025 clinical trial comparing oral tofacitinib and methotrexate demonstrated that tofacitinib yielded faster and more sustained regrowth in moderate-to-severe cases.
Another exciting addition is ritlecitinib, a selective JAK3/TEC kinase inhibitor, currently being studied for alopecia universalis. It has shown rapid and durable hair regrowth in patients with longstanding hair loss.
Outside of JAKs, researchers are also investigating topical dithranol, low-dose oral minoxidil (LDOM), and dual-targeted biologics for patients with coexisting inflammatory diseases.
This new wave of therapeutics is giving patients, especially those with long-standing or relapsing AA, real hope. But more studies are needed to understand long-term safety, optimal dosing, and resistance patterns—especially in pediatric and diverse populations.
Advances in Diagnosis and Prognostic Tools
While treatment breakthroughs are reshaping how Alopecia Areata (AA) is managed, early diagnosis and accurate prognostication remain crucial for personalized care. Recent research has focused on enhancing clinical tools to detect AA earlier, identify poor prognosis indicators, and track disease progression with greater precision.
One significant development is the increased use of trichoscopy and dermoscopy, which allow dermatologists to magnify and visualize specific hair and scalp features—like exclamation mark hairs, black dots, and yellow dots. These markers are increasingly being validated for disease activity scoring and treatment monitoring.
In a 2025 comparative study, dermoscopic patterns were found to be strongly associated with prognostic outcomes, with certain patterns indicating a higher risk of chronic or relapsing disease. This makes non-invasive diagnostic imaging an essential addition to clinical exams.
Another critical tool is the Severity of Alopecia Tool (SALT) score, which quantifies scalp hair loss and helps standardize treatment evaluation. While widely used, enhancements are underway to improve sensitivity to partial regrowth and patchy involvement.
Beyond clinical tools, genetics is offering new diagnostic insights. For example, the presence of AIRE gene mutations and filaggrin deregulations have been linked to treatment resistance and immune dysregulation. These discoveries open the door to biomarker-driven care, enabling early identification of patients likely to benefit from targeted therapies like JAK inhibitors.
Incorporating these tools into practice not only improves diagnostic accuracy but also empowers clinicians to make informed decisions about prognosis and treatment planning—ultimately leading to more personalized, proactive management.
Psychological Impact and Quality of Life in Alopecia Areata
Alopecia Areata (AA) may not cause physical pain, but its emotional and psychological effects are often profound—and often underestimated. As research increasingly reveals, the visible nature of AA-induced hair loss, especially on the scalp, eyebrows, and eyelashes, can significantly impact self-image, mental health, and social functioning.
Recent studies have shown that patients with AA are at higher risk for depression, anxiety, social isolation, and even post-traumatic stress disorder (PTSD) symptoms. A 2025 study from Japan revealed that perceived stigma was one of the strongest predictors of psychological distress in adults with AA, underscoring the need for psychosocial interventions alongside medical treatment.
In response, researchers and clinicians have developed tools to assess the quality of life (QoL) in AA patients. One major advancement is the 2025 Brazilian adaptation and validation of the Alopecia Areata Quality of Life Index (AA-QLI-BRA). This instrument allows for a culturally nuanced assessment of how hair loss affects patients emotionally, socially, and psychologically.
Importantly, pediatric patients are also uniquely vulnerable. Children with alopecia, especially when comorbid with conditions like atopic dermatitis, often experience bullying and self-esteem challenges. Case reports emphasize the importance of integrating mental health screening and support into treatment protocols for younger populations.
Addressing AA’s psychological impact is not just a matter of empathy—it’s a clinical necessity. Treating the hair loss without recognizing its emotional burden risks delivering incomplete care. As research makes clear, holistic treatment must consider the patient’s mind and identity, not just their scalp.
Pediatric and Gender-Specific Considerations in Alopecia Areata
Alopecia Areata (AA) affects individuals across all ages and genders—but children and women often experience unique clinical and emotional challenges that require tailored research and care approaches.
Pediatric Perspectives
In children, AA frequently coexists with atopic disorders like eczema or asthma, suggesting a broader dysregulation of the immune system. A 2025 case study from Japan described successful treatment of two pediatric patients with alopecia universalis and atopic dermatitis using baricitinib, a JAK inhibitor previously limited to adult use. These findings point toward emerging safe-use protocols for children, though long-term safety data remains limited.
Psychologically, children with AA face intense social pressure, bullying, and isolation, especially in school settings. Hair loss can disrupt social development and academic confidence, making early diagnosis and mental health screening essential components of pediatric dermatologic care.
Gender-Specific Findings
Among women, especially those of African descent, traction alopecia can be misdiagnosed or overlap with AA, complicating treatment strategies. A 2025 study noted that 21% of alopecia patients were misclassified initially, highlighting the importance of ethnically-informed diagnostic tools.
Additionally, AA is often more psychologically distressing in women due to societal expectations about hair and femininity. Recent patient surveys conducted within the UK’s NHS system revealed delays in diagnosis and referral, which many patients attributed to gender bias and underestimation of the disease’s impact.
As research becomes more inclusive, future therapies and diagnostic models must continue to reflect the biological, cultural, and psychological diversity among AA patients.
Conclusion & Future Outlook
The field of Alopecia Areata research is evolving faster than ever before. From breakthroughs in immunomodulatory treatments like JAK inhibitors to deeper understandings of the psychological and genetic complexities of the disease, the momentum is undeniable.
Where once patients were limited to unpredictable regrowth using corticosteroids or topical solutions, today’s treatments offer targeted, systemic therapies that address the underlying immune dysfunction. JAK inhibitors like baricitinib, tofacitinib, and ritlecitinib are transforming patient outcomes—especially in severe cases like alopecia universalis. Equally promising are advancements in diagnostic tools, including dermoscopy and trichoscopy, which enable earlier and more accurate detection of disease activity and progression.
Research is also finally recognizing the full human experience of living with AA. Quality-of-life measures, stigma studies, and pediatric-focused investigations are helping shape holistic treatment models that address both the physical and emotional toll of hair loss.
Yet, despite this progress, several challenges remain. Accessibility to advanced therapies, long-term safety data (especially in children), and disparities in diagnosis—particularly among women and ethnic minorities—need urgent attention. As more is uncovered about the genetic and environmental contributors to AA, the potential for personalized medicine becomes more tangible.
Looking ahead, we can expect continued focus on:
Biologic agents that target multiple immune pathways
Microbiome studies exploring skin and gut health connections
Patient-driven research, including real-world data on treatment outcomes
Digital diagnostic tools powered by AI and imaging analysis
Ultimately, the future of alopecia areata care lies in precision, empathy, and access. Whether you’re a patient, practitioner, or researcher, staying informed on the latest research empowers you to make proactive, evidence-based decisions.
References
Alkhalifah, A., Alsantali, A., Wang, E., McElwee, K. J., & Shapiro, J. (2010). Alopecia areata update: Part I. Clinical picture, histopathology, and pathogenesis. Journal of the American Academy of Dermatology, 62(2), 177–188.
https://www.sciencedirect.com/science/article/abs/pii/S0190962209013632
Kennedy Crispin, M., Ko, J. M., Craiglow, B. G., Li, S., & King, B. A. (2016). Safety and efficacy of the JAK inhibitor tofacitinib in treatment-resistant alopecia areata. JCI Insight, 1(15), e89776.
https://pmc.ncbi.nlm.nih.gov/articles/PMC5033755/
Villasante Fricke, A. C., & Miteva, M. (2015). Epidemiology and burden of alopecia areata: A systematic review. Clinical, Cosmetic and Investigational Dermatology, 8, 397–403.
https://www.tandfonline.com/doi/full/10.2147/CCID.S53985
King, B., Guttman-Yassky, E., Peeva, E., et al. (2022). Two randomized trials of baricitinib for alopecia areata. New England Journal of Medicine, 386(18), 1687–1699.
https://www.nejm.org/doi/full/10.1056/NEJMoa2110343
Muratani, S., Sato, E., & Imafuku, S. (2025). Two pediatric cases of alopecia universalis with atopic dermatitis successfully treated with baricitinib. JAAD Case Reports.
https://www.sciencedirect.com/science/article/pii/S2352512625002875